by admin | Nov 2, 2015 | Uncategorized
Ketamine May Reduce Chronic Pain in Adolescents

Subanesthetic ketamine infusions are a safe and effective way to relieve chronic pain in adolescents, a new study suggests.
Ketamine, a Schedule III drug, has been used successfully to treat various chronic pain syndromes in adults, according to researchers from Sheikh Zayed Institute for Pediatric Surgical Innovation, Children’s National Health System, in Washington, D.C., who conducted a longitudinal case series to determine the feasibility of ketamine injections in an outpatient setting.
“Our purpose was to look at the clinical outcomes related to our adolescents who were receiving what we considered subanesthetic dosing of ketamine,” said study author Kathy Ann Sheehy, CNS, a nurse specialist at the hospital.
The study included 63 adolescents with chronic pain conditions such as complex regional pain syndrome (CRPS), fibromyalgia and headache, and were treated in the hospital’s tertiary outpatient interdisciplinary Pain Medicine Care Complex from January 2013 to April 2014. The patients received 111 treatments (277 ketamine infusions; maximum dose of 1 mg/kg per hour) during the study period. They were divided into two groups: CRPS (n=23) and all other chronic pain syndromes (n=40). Main outcome measures were self-reported pain scores using a numeric rating scale and morphine-equivalent intake.
The researchers found that ketamine significantly decreased pain scores in 37% of the injections administered. A reduction of 20% or greater was considered significant. Patients with CRPS experienced the greatest reduction compared with the other chronic pain syndromes (P=0.029). The researchers noted that the ketamine infusions did not change the overall morphine-equivalent intake (P=0.3).
“When we looked at the difference between the types of pain syndromes, CRPS was the one that was the most statistically significant as a pain syndrome for reduction in pain scores and reduction in opioid use,” Ms. Sheehy said. “[With] the other pain scores, although overall there was a reduction, we didn’t see a reduction in headaches or other types of complex pain syndromes.”
An analysis of comorbidities showed that:
- 23% of the patients had psychiatric/psychological disorders (e.g., anxiety, depression, bipolar disorder);
- 10% had a history of trauma;
- 10% had postural orthostatic tachycardia syndrome (POTS);
- 7% had diabetes mellitus;
- 7% had a malignancy; and
- 5% had sickle cell disease.
The researchers found that the patients with POTS and trauma experienced the greatest pain reduction and chronic headache patients had the smallest decrease. “Our assumption for that is that both of those are autonomic sympathetic conditions, and most of our CRPS kids actually had trauma,” Ms. Sheehy said.
No adverse events were reported and the ketamine injections were well tolerated, according to the study authors. They said more research on complex pain syndromes, especially CRPS in adolescents, is needed.

by admin | Aug 31, 2015 | Uncategorized
Comprehensive Management Of Chronic Knee Pain
Knee pain is a very common complaint that can be debilitating when severe. A proper evaluation must begin with a thorough history and physical examination.
If the patient is not a surgical candidate, there are several conservative treatment options—such as physical therapy for retraining of proper mechanics, kinesiology taping to improve proprioception, acupuncture and chiropractic treatment—that may alleviate the patient’s symptoms (Figure 1).

Depending on the nature of the pain, a variety of analgesic medications may be prescribed, including anti-inflammatory drugs, membrane-stabilizing agents and in severe cases, opioid analgesics. Unfortunately, these medications may not significantly reduce the pain and their long-term compliance may be limited by untoward side effects. Additionally, many patients have intractable chronic pain after more invasive treatment options such as a total knee arthroplasty (TKA). Studies have reported that 20% of patients undergoing TKA have persistent postsurgical pain.1 These patients often present to the pain clinic frustrated by the failure of conservative and possible surgical interventions. Fortunately, depending on the pain generator, there is a wide array of interventional treatment options that can be implemented (Figure 2).

History and physical
Diagnostic workup (ultrasound, x-ray, MRI, NCS/EMG)
Possible surgical candidate?
If yes, consider early orthopedic referral
If no, consider conservative management
Manual therapy (PT, chiropractor/DME)
Analgesics (ibuprofen, NSAIDs)
Behavioral, psych (biofeedback, relaxation techniques)
Figure 1. Conservative treatment algorithm.
DME, durable medical equipment; EMG, electromyography; MRI, magnetic resonance imaging; NCS, nerve conduction study; NSAID, nonsteroidal anti-inflammatory drug; PT, physical therapy
Failed conservative treatment
Phase 1
Image-guided knee steroid/hyaluronic acid injection
Image-guided knee stem cell/PRP injections
Phase 2
Saphenous and lateral femoral cutaneous nerve block; RFA if successful
Femoral nerve block, RFA if successful
Lumbar sympathetic plexus block (L2, L3); RFA if successful
Genicular nerve block; RFA if successful
Lumbar SCS trial; permanent implant if successful
PNS trial; permanent implant if successful
Phase 3
Refer back to orthopedic surgeon for reevaluation
Figure 2. Nonsurgical knee pain.
PNS, peripheral nerve stimulation; PRP, platelet-rich plasma; RFA, radiofrequency ablation; SCS, spinal cord stimulation
Evaluation
The primary nerve innervation of the knee arises anteriorly from the femoral nerve and posteriorly from the sciatic nerve. These nerves give rise to a number of smaller branches that provide sensation to a variety of specific regions around the knee (Figure 3). The saphenous nerve branches from the femoral nerve and provides sensation over the distal aspect of the medial two-thirds of the thigh. The lateral one-third of the distal thigh is supplied by the superficial femoral cutaneous nerve. The superior medial, inferior medial, and middle genicular nerves arise from the tibial nerve—the medial division of the sciatic nerve. The superior lateral, inferior lateral, and recurrent tibial genicular nerves arise from the common peroneal nerve—the lateral division of the sciatic nerve.2

Figure 3. Innervation of the knee.
A thorough history and physical can aid the clinician in developing a focused differential diagnosis and effectively managing the patient with knee pain. Specific location of the pain, cause of the pain, duration of symptoms, alleviating and/or exacerbating factors, associated ipsilateral back and/or hip pain, and the outcome of any previous interventions should be investigated. The physical exam should always begin with inspection of the knee to assess for signs of gross deformity, edema, or cellulitis. Provocative exam maneuvers such as the valgus/varus stress, anterior/posterior drawer, Lachman’s test, McMurray’s test, and the patellar grind test may provide a great deal of information whether positive or negative. If bony etiology is suspected, imaging should include an x-ray of the knee. However, if soft tissue pathology is suspected, an ultrasound or a magnetic resonance imaging scan of the knee may be more appropriate. Furthermore, given that it is common for knee pain to be a manifestation of referred back or hip pain, imaging of these regions as well as electrodiagnostic studies may be appropriate. Electrodiagnostic studies also should be completed if there is any concern for neuropathy. Correlating the patient’s symptoms and physical exam findings with abnormal diagnostic test results can help to condense the differential diagnosis and aid in tailoring a treatment plan.3
Current Evidence for Interventional Therapy
There is a growing body of literature that supports the use of a variety of interventional procedures in the management of knee pain. Raynauld et al demonstrated improved pain relief with intraarticular steroid injection versus saline over a 2-year period with repeated injections every 3 months.4 Neustadt et al showed that intraarticular hyaluronic acid injections brought about some symptomatic pain relief compared with placebo.5 A study by Choi et al revealed that radiofrequency ablation of the superior medial, superior lateral, and inferior medial genicular nerves produced significant pain relief in patients with knee osteoarthritis.6 Wakitani et al demonstrated repair of articular cartilage defects following intraarticular injection of human autologous mesenchymal stem cells.7
Ultrasound Versus Fluoroscopically Guided Injections

Figure 4. Knee ultrasound.
Arrowheads, medial collateral ligament
Medial meniscus
Distal hip adductor muscles can be seen at the top of the image.
Incorrect placement of injectate within the knee can lead to increased pain and decreased therapeutic benefit. The literature suggests that there is an increased rate of successful intraarticular placement using image guidance compared with blind injections (ie, using surface anatomic landmarks). In light of this, ultrasound and fluoroscopy are both frequently used to perform interventional procedures for knee pain. Each has advantages and disadvantages with respect to a given procedure. Fluoroscopy provides better visualization of the knee joint, which improves the likelihood of successful intraarticular injection. Given the relatively radiopaque appearance of periosteum and hardware from prior TKA, this is ideal for genicular nerve blocks. However, the patient is subjected to radiation exposure with its usage. Ultrasound allows for better visualization of soft tissue structures, which can dramatically improve the success rate of peripheral nerve and bursa injections in this region (Figure 4). The normal characteristic appearance of various anatomic structures in the region of the knee aid the interventionalist in target localization. Given the real-time dynamic nature of this imaging modality, the needle tip and/or injectate can be easily visualized for both intra- and extraarticular injections to confirm accurate location.8,9 For ease of access into the intraarticular joint space, we recommend performing procedures with the patient in the supine position with the knee maximally flexed to approximately 135 degrees. It is important to note that ultrasound is user-dependent, which makes for more variable results.
Interventional Procedures
The following is a list of interventional procedures that are commonly performed in the treatment of chronic knee pain:
Intraarticular knee injections: steroids, hyaluronic acid, traumeel, platelet-rich plasma (PRP), and mesenchymal stem cells (Figure 5).
Extraarticular knee injections: steroids, traumeel, PRP, and mesenchymal stem cells.
Trigger-point injections.
Peripheral nerve blocks: saphenous, superficial femoral cutaneous, genicular nerves (Figure 6).
Radiofrequency ablation: saphenous, superficial femoral cutaneous, genicular nerves.
Lumbar sympathetic plexus block (typically at L2 and/or L3 level).
Peripheral nerve stimulation: saphenous, superficial femoral cutaneous.
Lumbar spinal cord stimulation: treatment of last resort.

Figure 5. Mesenchymal stem cells.
Regenerative therapy can include platelet-rich plasma and stem cells. Mesenchymal stem cells may be procured from autograft bone marrow and
image

Figure 6. Peripheral nerve stimulation.
The patient is a 19-year-old female collegiate softball player who failed multiple orthopedic knee surgeries and was unable to participate in athletic activities. Following placement of peripheral field stimulation of the knee, she was able to return to play.
Courtesy of Dr. William S. Rosenberg, Center for the Relief of
References
Beswick AD, Wylde V, Gooberman-Hill R, et al. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1).
Jacobson JA. Introduction. In: Jacobson JA, ed. Fundamentals of Musculoskeletal Ultrasound. Philadelphia, PA: Saunders; 2007:1-14.
Jacobson JA. Knee ultrasound. In: Jacobson JA, ed. Fundamentals of Musculoskeletal Ultrasound. Philadelphia, PA: Saunders; 2007:224-263.
Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee. Arthritis Rheum. 2003;48:370-377.
Neustadt D, Caldwell J, Bell M, et al. Clinical effects of intraarticular injection of high molecular weight hyaluronan (Orthovisc) in osteoarthritis of the knee: a randomized, controlled, multicenter trial. J Rheum. 2005;32:1928-1936.
Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011;152:481-487.
Wakitani S, Imoto K, Yamamoto T, et al. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. J Osteo Res Soc Inter. 2002;10:199-206.
Waldman SD. Pain Management. Philadelphia, PA: Saunders; 2011.
Hurdle M-FB. Ultrasound-guided knee injections. In: Narouze SN, ed. Atlas of Ultrasound-Guided Procedures in Interventional Pain Management. New York, NY: Springer; 2011:331-335
BY: Tory McJunkin, MD
Co-founder
Arizona Pain Specialists
Scottsdale, Arizona
Paul Lynch, MD
Co-founder
Arizona Pain Specialists
Scottsdale, Arizona
Jarron Tilghman, MD
Physical Medicine and Rehabilitation Physician
Rockhill Orthopaedic Specialists
Kansas City, Missouri
Patrick Hogan, DO
Anesthesiologist, interventional pain physician
Arizona Pain Specialists
North Phoenix, Arizona
Adam Wuollet, MD
Anesthesiologist, interventional pain physician
Arizona Pain Specialists
Phoenix, Arizona
Edward Swing, PhD
Research Director
Arizona Pain Specialists Scottsdale, Arizona
by admin | Aug 3, 2015 | Uncategorized
It has been estimated that 1 in 4 people in the US suffer from some form of chronic pain in their lifetime. The duration of this pain differs from person to person, spanning several weeks to many years.
Many sufferers of long-term chronic pain can have their daily wellbeing severely affected if treatments fail to offer appropriate levels of pain relief.
Of the more than 1.5 billion people worldwide said to suffer from chronic pain, the most common area affected is the lower back. The frequency of this is 23-26% of the global population.
Not surprisingly, this has been a hot area of research, which has produced treatment options from opioids to surgery. Opioids, while very effective for analgesia, can produce unwanted long term problems like dependence for chronic pain patients.
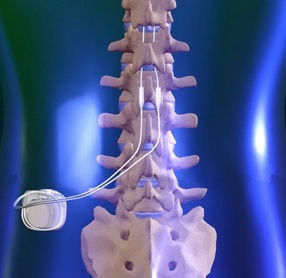
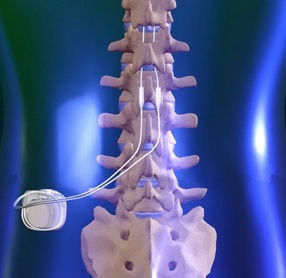
For this reason, surgical options are frequently presented for long term chonic pain patients. One such technique is spinal cord stimulation therapy (SCS), where pulses are delivered to the spinal cord by a small device implanted under the skin, emitting a form of paresthesia. As many as 50,000 patients in the US undergo SCS ever year to combat chronic pain.
Paresthesia is a sensation akin to tingling and is a result of SCS. When a device is turned on, an electrical current interrupts the pain signal being sent to the brain. Although a patient’s pain is not cured, SCS hopes to offer some temporarily relief.
Although SCS has been shown to reduce pain, many patients find the paresthesia that accompanies this to be uncomfortable.
This was to be the catalyst for scientists to develop a new form of SCS, one which still alleviates pain but reduces the effects of paresthesia in patients.
Traditional SCS uses frequencies of 40-60 hertz. Scientists decided to intensify this and use high-frequency pulses capable of delivering up to 10,000 hertzes. The new treatment has been named HF10.
Prof. Leonardo Kapural, lead study author and professor of anesthesiology at Wake Forest University School of Medicine and clinical director at Carolinas Pain Institute at Brookstown in Winston-Salem – both in North Carolina – believes the research to be the first of its kind.
“This is the first long-term study to compare the safety and effectiveness of high-frequency and traditional SCS therapy for back and leg pain,” he explains.
Scientists examined 171 patients with chronic back or leg pain, of whom 90 received HF10 therapy and 81 were treated with traditional SCS.
After 3 months, researchers found 85% of back pain and 83% of leg patients receiving HF10 therapy reported a 50% reduction in pain or greater. These patients also reported no experience of paresthesia.
In contrast, patients undergoing SCS reported less effective results. Only 44% of back pain patients and 56% leg patients experienced a minimum 50% reduction in pain.
The study ran over a 12-month period and found HF10 to be more effective compared with traditional SCS. More than half of the HF10 sample group reported being “very satisfied” with the outcome, compared with just 32% of patients who received traditional SCS.
Prof. Kapural hopes this research will be an important step toward treating chronic pain.
SCS represents an alternative for those patients who wish to avoid surgery or drugs such as opioids. According to a 2011 report, at least 100 million adult Americans suffer from chronic pain. In the same report, it was also estimated that chronic pain costs society between $500-635 billion a year.
Dr. Hanna has many years of experience performing SCS procedures for chronic pain patients. To learn if this procedure might be right for you, please make an appointment with Dr. Hanna at the Florida Spine Institute in Clearwater, FL. His contact information can be found here.

by admin | Jul 16, 2015 | Uncategorized

If you’re looking for natural ways to fight the aches, stiffness and inflammation of fibromyalgia, supplements can be a powerful weapon against symptoms. From vitamin D to brown seaweed extract, an arsenal of tools can help reduce pain. Here, experts reveal what works and why…
If you’re not including fibromyalgia-fighting supplements as part of your pain-management regimen, you could be missing out.
“The right supplements can help muscles relax, which leads to pain reduction, or even prevent pain altogether,” says fibromyalgia expert Jacob Teitelbaum, M.D., director of the Fatigue & Fibromyalgia Practitioners Network and author The Fatigue and Fibromyalgia Solution (Avery).
But when you’re standing in the supplement aisle, it’s hard to figure out which live up to their hype.
Read on for expert advice on the top 6 supplements for relieving fibro pain and other symptoms.
1. Vitamin D
The “sunshine vitamin” isn’t only good for building bones.
It can help fight fibro pain and fatigue, too, according to a 2014 study published in the journal Pain.
For the study, 30 women with fibromyalgia – who were also deficient in vitamin D – were divided into two groups. The treatment group received oral vitamin D supplements for 20 weeks. The control group received a placebo.
Starting after just one week, the treatment group showed improved physical functioning, had less morning fatigue than the placebo group and reported a marked reduction in pain.
The body produces vitamin D when skin is directly exposed to the sun – our best source. But some people don’t produce enough of the nutrient, according to the National Institutes of Health. These include women who are older, dark-skinned or obese.
People with certain disorders, including celiac or Crohn’s disease – as well as those who aren’t exposed to ample sunlight (or who wear sunscreen) – are also likely to be deficient. (Read about 11 natural remedies for Crohn’s management.)
Because few foods contain vitamin D, swallowing supplements is the easiest way to ensure you get enough.
The government’s daily recommendation of vitamin D is 600 international units (IU) for anyone 1 to 70 years old, and 800 IU for people 71 and up – to a maximum of 4,000 IU per day, according to the National Institutes of Health.
But ask your doctor how much you should take to combat your fibro symptoms.
2. Fish Oil
Thanks to its omega-3 fatty acids, fish oil has terrific anti-inflammatory properties, which can help reduce fibro pain.
It reduces the body’s production of inflammatory hormones (prostaglandins), says Nehad Soloman, M.D., a board-certified rheumatologist for Valley Arthritis Care in Arizona. And that may mean less stiffness or fewer tender joints.
Dr. Soloman suggests choosing a mercury-free brand (check the label), although fish oil supplements are considered safe.
Take 1 or 2 capsules (or 1 or 2 tablespoons) daily to reduce inflammation and boost your immunity, recommends the University of Maryland Medical Center. But check with your doctor first – especially if you take blood-thinning medications, such as aspirin or warfarin (Coumadin).
3. SAMe
S-Adenosyl methionine, more commonly known as SAMe, is a synthetic form of a compound the body naturally produces.
We need it for proper immune function, and it plays a role in forming cartilage and our DNA, Dr. Soloman says.
As we age, our bodies produce less of it, which may explain the increased aches after your 40th birthday. Taking a SAMe supplement not only lessens chronic pain, it also can boost your spirits. These 5 other natural mood-lifters help too.
“SAMe assists in the production and breakdown of neurotransmitters, such as serotonin, norepinephrine and dopamine – brain hormones that influence and regulate moods,” Dr. Soloman says.
In fibro studies, the recommended dosing is 400 mg twice a day for six weeks, starting with a lower dose (about 200 mg daily) and increasing gradually to avoid stomach upset, according to the University of Maryland Medical Center. But dosing varies by patient, so ask your doctor.
4. Ribose
Tight muscles are a common cause of fibro pain. To relax and release, muscles need energy, Dr. Teitelbaum says. And that’s where ribose supplements come in.
Ribose, a simple sugar, can increase energy by an average of 61% – and cut the pain experienced by fibromyalgia sufferers by an average of 15.6%, according to a 2012 study Dr. Teitelbaum led, published in The Open Pain Journal.
“The energy-building benefit of ribose directly improved the debilitating symptoms of this condition,” Dr. Teitelbaum says.
Dr. Teitelbaum recommends a 5 g dose three times a day.
5. Magnesium
This mineral is a major player in every body part.
Not only is it credited with keeping the heart, kidneys and bones strong, it also helps us avoid muscle spasms, weakness and back pain, Dr. Teitelbaum says.
Women with fibromyalgia may be deficient in magnesium, studies suggest. And magnesium may help relieve fibro pain and other symptoms.
For example, researchers from Ajou University School of Medicine in Korea analyzed hair samples from 166 women – including 44 with fibromyalgia. The hair from the fibromyalgia group contained significantly lower amounts of magnesium than that of the healthy women, according to the 2011 study.
Researchers at Acıbadem University Medical School in Istanbul, Turkey, also found that women diagnosed with fibromyalgia were likely to have “significantly lower” magnesium levels than women who didn’t have the disorder. But those who then took 300 mg/day of magnesium citrate for 8 weeks reported a reduction of “tender points” and other fibromyalgia symptoms, according to their 2013 study.
Magnesium is found in green leafy vegetables, pumpkin and sunflower seeds, 100% wheat bran cereal and raw spinach.
But these foods are a good source only if you eat them raw. Half of the minerals’ benefits are lost when cooked.
Normal daily recommended dosage for adult women is 280 to 300 mg per day, taken with meals, says the Mayo Clinic.
But if you have kidney disease or are taking medication, talk to your doctor before taking magnesium. Magnesium can interact with certain medications, including high blood pressure medicines and antibiotics, the University of Maryland Medical Center says.
6. Brown Seaweed Extract
You may not be familiar with these capsules, but this supplement is one to look for.
“It’s showing great promise in the fight against chronic pain,” Dr. Soloman says.
In fact, taking 1,000 mg of brown seaweed extract daily can reduce joint pain and stiffness by 52%, according to a 2011 study from Australia’s Centre of Health and Wellbeing, published in the journal Biologics.
Even better: These benefits kicked in after just one week, so you don’t have to wait long to find out if it’s working for you.
Supplement Smarts
Check with your doctor before taking these or other supplements.
“Like prescription drugs, it’s possible to take too much. And many supplements have side effects,” says David Pisetsky M.D., Ph.D., a professor of immunology at Duke University Medical Center in Durham, N.C.
Questions to ask your doctor include:
1. What’s the right dosage for me?
2. Should I take it with food?
3. What time of day should I take it?
4. Will this supplement interact badly with my prescriptions?
5. Does it have side effects that might mimic or aggravate my fibro symptoms (such as depression or sleep difficulties)?
For more expert advice and information, visit Lifescript’s Fibromyalgia Health Center.
Also, visit these other resources for more support:
The National Institutes of Health: Information and resources from the U.S. government’s medical research agency.
The American Fibromyalgia Syndrome Association: This group’s mission is to fund scientific studies on fibromyalgia.
Fibromyalgia Network: A nonprofit that offers information about the disease from top fibromyalgia clinicians and researchers.

by admin | Jun 30, 2015 | Uncategorized
A clinical study conducted by researchers at the Leiden University Medical Center in The Netherlands evaluated the efficacy of a multi-day infusion regimen of intravenous ketamine for the treatment of Chronic Regional Pain Syndrome Type 1. This double blind, placebo-controlled study validated intravenous ketamine as a treatment for CRPS-1, which historically responds poorly to standard pain treatment. Sixty CRPS-1 patients were randomized into groups to undergo infusion therapy for 4.2 days with intravenous ketamine or placebo. The researchers measured pain levels in these patients using a numerical pain score assessment. They found that pain scores over the 12 week study period in patients receiving ketamine were significantly lower compared to those that received placebo (P<0.001). Importantly, after the 12th week, statistical significance between the two groups was lost, indicating that the infusion regimen that the researchers used is not a permanent fix for CRPS-1. Nonetheless, it did provide relatively long lasting relief in a patient population that is desperate for more effective therapies. Intravenous ketamine could be the answer that they’re looking for.
Future studies should focus on the optimal dose of intravenous ketamine and possible synergistic combination drugs to enhance the efficacy of this treatment option for the treatment of chronic pain conditions, like CRPS. A new combination ketamine infusion therapy is offered at the Florida Spine Institute that might just be the answer for long lasting analgesic efficacy. To find out if this procedure is right for your chronic pain, please make an appointment to see Dr. Ashraf Hanna, an expert pain management doctor with significant experience using intravenous ketamine. It is our goal at the Florida Spine Institute to conduct the cutting edge research necessary to eradicate CRPS once and for all.
Full Citation:
Sigtermans, M.J., van Hilten, J.J., Bauer, M.C., Arbous, M.S., Marinus, J., Sarton, E.Y., Dahan, A., 2009. Ketamine produces effective and long-term pain relief in patients with Complex Regional Pain Syndrome Type 1. Pain 145, 304-311.