by admin | Jan 14, 2015 | Uncategorized
Dealing with Fibromyalgia on a daily basis is a trial that many have to deal and battle with in their life. Fibromyalgia is a chronic pain disorder that causes pain all throughout the body such as the muscles, and joints. The pain is intense especially when pressure is applied to these pressure points also known as tender points. These tender points are at the shoulders, back of the neck, hands, knees, around the neck, and the hip joints. Research has found that the illness may be hereditary being passed down the family line and more women than men have the disorder. Treating Fibromyalgia by providing relief of the pain and other symptoms of the illness is a tricky task but it can be done. Exercising with Fibromyalgia takes time and effort to gain relief from the pain, along with improving sleep, and alleviating other symptoms of the disorder. Weight loss may help with reducing additional pain in the body such as pain in the legs, cardiovascular functioning, Lack of exercise and conditioning of the body brings on symptoms of increased sensitivity to pain, along with osteoporosis, degenerative disc disease (DDD), rheumatoid arthritis (RA), lower back pain, weakened muscles in the back, lumbar, pelvis area, and thighs. Patients who suffer with Fibromyalgia need to exercise a minimum of two times a week for a minimum of 25 minutes each time of exercise. Doing this may help to reduce symptoms of the illness. If you’re just starting out with exercising it is best to start out slow by picking out a low to moderate intensity of exercise such as walking in the mall, water aerobics, swimming, yoga, tai chi, etc. As time goes by then increase the amount of time and intensity when you feel ready to do that type of move.
1. Try warm water aerobics in the pool which is the perfect environment to relieve pain and stiffness in the body. The Arthritis Foundation Aquatic Program is a program that allows patients to exercise gently in the warm water which in turns helps to build up their strength and ability to be more flexible. Many patients who participate in this exercise activity will find their pain will have decreased and lessened stiffness.
2. Expand your mind and body with Yoga. Yoga allows the person to train their mind, body and spirit This type of exercise fits within the alternative and complementary medicine. There are many different types of physical yoga or also known as Hatha (poses). The different types of yoga are such as Bikram which focuses on stamina and purification using heated rooms that are over 100 degrees, or Vinyasa/power yoga which helps to increase stamina, strength and flexibility.
3. Look into applying the mind-body practices Tai Chi and Qigong into your fitness schedule. Both of these practices originated in ancient China. Anyone of any age and health condition can do these of type of movements. Tai Chi which is an exercise focused on easy movement mobility, breathing and improving relaxation. Tai Chi is a low impact type of aerobics with the focus on reducing pain, and stiffness. With Tai Chi there are 12 movements with half are basic and the other half are advanced movements. Qigong reduces stress, improves the immune system, lowers blood pressure, improves overall stamina, cardiovascular, and digestive function.

by admin | Jan 14, 2015 | Uncategorized

Fibromyalgia is a musculoskeletal disorder involving widespread pain, fatigue, sleep problems and mood disturbances. It is not known what definitively causes this disorder, and right now, there is no cure. Treatments available, though, including over-the-counter supplements, to help relieve symptoms. If you have fibromyalgia, talk to your health care provider before taking any supplements to make sure they are safe and appropriate for you to use.
Magnesium is a mineral that is needed by every organ in the human body. The University of Maryland Medical Center states that this mineral helps build strong teeth and bones; activates enzymes; plays a role in producing energy; and helps regulate calcium, copper, zinc and other nutrient levels. A 2008 study by O.F. Sendur and colleagues, published in the journal “Rheumatology International,” found that individuals with fibromyalgia had significantly lower magnesium levels. According to UMMC, preliminary studies show that magnesium and malic acid may help relieve pain and tenderness in fibromyalgia patients when taken for at least two months. Study results have been mixed, and more extensive research needs to be done.
The amino acid tryptophan is converted into 5-hydroxytryptophan, or 5-HTP, and then converted into serotonin. Serotonin affects mood and behavior, and it is thought that 5-HTP may improve sleep, mood, anxiety and pain sensation, states UMMC. Individuals with fibromyalgia are sometimes prescribed antidepressants because lower levels of serotonin have been associated with the condition. According to UMMC, while not all studies have found the same results, some studies showed that 5-HTP eased fatigue, morning stiffness, pain and anxiety associated with fibromyalgia. Talk with your doctor before using this supplement, especially if you are already taking an antidepressant.
The compound S-adenosylmethionine, or SAMe, is naturally found in nearly every tissue of the body. It helps break down neurotransmitters like dopamine, serotonin and melatonin, among other things. When used as a supplement, SAMe may help relieve some symptoms of fibromyalgia, states Rxlist.com. It has been used to help treat depression and osteoarthritis and can help with similar symptoms in sufferers of fibromyalgia. UMMC states that injectable SAMe has been effective in helping reduce depressed mood, pain and fatigue, along with joint pain, in individuals with fibromyalgia. Talk to your doctor before using SAMe to treat any medical condition.
Along with these supplements, there are medications that may be helpful in easing symptoms of fibromyalgia. According to MayoClinic.com, other treatments include anti-seizure drugs to help reduce nerve pain, analgesics to loosen stiff joints and provide pain relief, and antidepressants to help with fatigue and depression. Talk therapy, getting enough sleep and regular exercise can also ease stress and provide fibromyalgia relief. What works for one patient may not be effective for another, so it is best to find what helps you the most.

by admin | Jan 13, 2015 | Uncategorized
If you’re living with fibromyalgia, simple steps you can do right now can help prevent a painful fibromyalgia flare.
For the 5 million Americans living with fibromyalgia, the discomfort that characterizes this condition never really goes away. But from time to time, sudden bouts of intense pain, fatigue, and other symptoms — known as fibromyalgia flares — will also occur. While there’s no definitive way to avoid occasional flares, you can be proactive and develop strategies to keep your symptoms in check, according to Sharon Ostalecki, PhD, a nationally recognized fibromyalgia patient advocate.
Preventing a Flare: Focusing on Self-Management
- Journaling. “Take 10 minutes every day to jot down things like what activities you did, what medication you started, sleep, or if you ate something new,” Ostalecki suggests. “Journaling is the key to discovering your flare triggers, so you can try to avoid them.” She notes that it can take up to 48 hours for an event to trigger a fibromyalgia flare-up, and if it’s not noted somewhere, you might not remember or recognize the correlation.
- Delegating and saying no. “Many people with fibromyalgia are perfectionists and like to do everything themselves, from all the cleaning to all the cooking,” says Ostalecki, who includes herself in this category. “But you have to learn to let others do things for you because even mild overexertion can lead to a severe flare-up.”
- Stress management. “Stress tightens you up, and when you have fibromyalgia, the muscles don’t let go,” Ostalecki explains. “Find something that reduces stress for you before it gets to that painful point. I like listening to books on tape, for instance.”
- Standing tall. Learning and maintaining proper posture is crucial to managing fibromyalgia, because posture errors that push the head too far forward or cause slouching can lead to muscle fatigue, followed by increased tension and pain.
- Proper diet. Protein intake is vital to those with fibromyalgia “because it’s the only macronutrient that builds and maintains muscle,” says Ostalecki, who earned her doctorate in nutrition. “A diet low in protein results in more nodules, more pain, and consequently more exhaustion.”
Preventing a Flare: Finding What Works for You
You can best assess whether a particular therapy is working by following these steps:
- Start only one new treatment at a time.
- See if you feel better when you use the treatment.
- Stop the treatment, and see if you get worse.
- Restart the treatment, and see if you improve again. If you do, you can be fairly confident that this treatment has a positive effect on you.
Preventing a Flare: Staying Positive, Outwardly Focused, and Upbeat
Finally, as hard as it may be, trying not to let fibromyalgia become the focus of your life is an important step in staying well and avoiding flares, says Ostalecki, who’s also executive director of H.O.P.E., a non-profit organization that works to increase fibromyalgia awareness. “Find something that brings you joy, whether it’s your dogs, your garden, your painting, or whatever,” she advises. Without such an emotional outlet, “chronic pain will become all you talk about, and that will impact your relationships.” Strained relationships bring more stress and likely more symptoms — exactly the outcome you want to avoid.
by admin | Jan 9, 2015 | Uncategorized
Introduction
Radiofrequency ablation is a term used when radio waves are used to produce heat to destroy tissue, usually a nerve. It has been used for several years with great success in patients who have abnormally fast heartbeats. More recently, it is being used to destroy tumors. It is a non-surgical option to treat your spine pain.
Spine pain is the second most frequent pain complaint. It occurs in 65 to 80 percent of the population at one time or another, and can be disabling and frightening. Its costs to society are great.
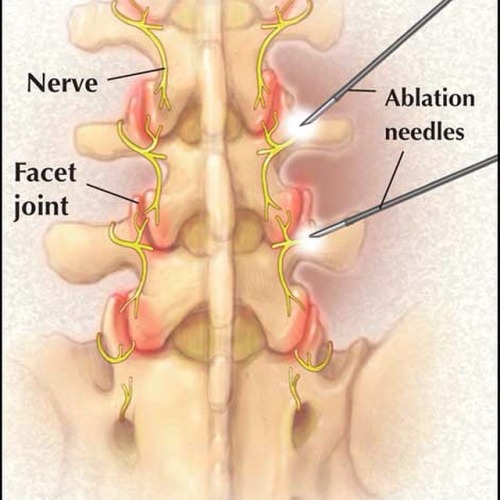
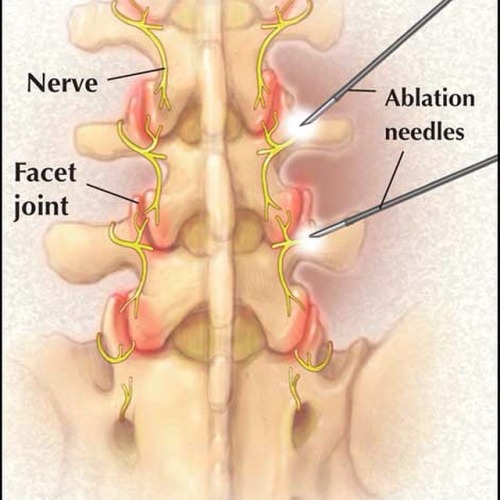
In the case of spinal pain, radiofrequency waves are transmitted through a needle placed into the facet joint under x-ray guidance. This procedure is also known as rhizotomy.
This guide will help you understand
- What parts of the spine are involved
- What is the surgeon is trying to achieve
- What happens during the procedure
- What are the possible complications
Anatomy
What parts make up the spine?
The spine is made up of three general parts. The top portion is the cervical spine and connects with the skull or cranium. The middle portion is the thoracic spine and is identified by the ribs that attach to each of the vertebrae. The lower portion is the lumbar spine. It connects with the pelvis at the sacrum.
The human spine is made up of 24 spinal bones called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
The vertebrae have discs that serve as cushions in between them. Each vertebra has two sets of bony knobs that meet between each vertebra. These form facet joints. The facet joints are located on the back of the spinal column in the lumbar and thoracic spine. In the neck, or cervical spine, they are located on each side of the vertebra. They are also called zygoaphophyseal or apophyseal joints.
A joint is where two or more bones are joined, allowing motion. Facet joints allow flexion or forward bending, and extension or backward bending, as well as rotation of your spine. The facet joints are synovial joints. This means that a capsule of soft tissue encloses them to help support it. It also makes fluid that lubricates the joint, like oil for the moving parts of a machine.
The surfaces of the joints are lined with cartilage. This allows joints to move or glide smoothly. The articular cartilage surface of the facet joint can become thin due to wear and tear. Bone spurs and enlargement of the joint can occur due to chronic inflammation and arthritis.
Nerves called medial branches supply facet joints. They carry the pain signals to the spinal cord. The signals eventually reach the brain where the pain is registered. Pain is a warning when the joint is irritated.
Rationale
What do surgeons hope to achieve with this procedure?
There are several structures in the spine that can be a source of pain. One of the most common sources is the facet joint. The joints can develop arthritis and cause acute and chronic pain. The pain may come and go depending on activity.
Facet joint pain as the cause of back pain can be determined by a facet joint injection. This is called a diagnostic injection, meaning the doctor uses it to help make a diagnosis. The physician using x-ray guidance will inject the facet joint(s) in question with a small amount of a combination of local anesthetic and cortisone. Relief of the acute or chronic problem while the joint is numb indicates that you will likely have a good response to radiofrequency ablation.
Radiofrequency ablation uses radio waves to produce heat to destroy the nerve(s) carrying the pain signals from the facet joint. Once the nerves carrying pain sensation from the joints are destroyed, your pain should be reduced. This should allow you to do more activity, and decrease your pain medications.
Preparation
How should I prepare for the surgery?
Your surgeon will discuss the preoperative guidelines. Follow your surgeon’s instructions. These instructions may include
- Do not eat or drink for at least six hours before the procedure. You will be able to take your usual medication with a small amount of water. If you have diabetes, do not take your insulin or diabetic pills until after the procedure
- You will need a driver to return home
- Do not take any aspirin or aspirin-containing medication at least eleven days before the procedure. They may prolong bleeding
- Wear loose fitting clothing that is easy to take off and put on
- Take a shower the morning of the procedure, using a bactericidal soap to reduce chances of infection
- Do not wear jewelry
Procedure
What happens during the procedure?
When the procedure is to begin, an IV will be started. This will allow the use of medications to help sedate you and make the procedure more comfortable. It is also important to have IV access for medications if you should have an allergic reaction during the procedure.
You should be awake for the procedure to help the doctor with correct placement of the electrode used for radiofrequency ablation. You will not be given a general anesthetic. The area to be treated will be cleaned and then numbed with a local anesthetic.
Using x-ray guidance, the doctor will place the needle in the proper facet joint. A microelectrode is then placed inside the needle. A small radiofrequency current is then sent to the medial branch nerve of the joint capsule for approximately 60 to 90 seconds. The procedure is done with sterile technique to minimize the risk of infection.
After the procedure, you will be taken to a recovery area. The nurses will monitor you and be sure you do not have an allergic reaction. You will be allowed to leave once you are stable.
Complications
What might go wrong?
This procedure is a safe, non-surgical treatment, and the risks for complications are low. However there are several complications that may occur during or after this procedure. No procedure is 100 percent foolproof. This article doesn’t provide a complete list of all the possible complication, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur. Some of the most common complications following radiofrequency ablation include
- Neuritis
- Neuroma
- Numbness-nerve damage
- Infection
- Allergic reaction
- Lack of pain relief
Neuritis
Neuritis is an inflammation of the nerve with pain and tenderness that lasts three to six weeks. This can occur in 10 to 15 percent of patients. Neuritis usually goes away by itself. If it doesn’t, the doctor can inject a local anesthetic along with a steroid into the nerve. Pulsed radiofrequency can also be used to help with the pain and inflammation.
Neuroma
A neuroma is a tumor from a nerve made of nerve cells and fibers. It forms around the area destroyed during radiofrequency ablation. The tumor can put pressure on the nerve and nearby tissue causing increased pain.
Numbness
Numbness caused by nerve damage can occur. Permanent numbness is also a possible complication.
Infection
Infections can also happen. Infections can involve the skin, or the joint and surrounding bone.
Allergic Reaction
Allergic reactions can occur since medications and sometimes contrast dye is used during the procedure. Anaphylaxis is an allergic reaction that is serious and can result in death.
Lack of Pain Relief
Even though a test block was beneficial, some patients have no pain relief from the procedure.
After Care
What should I expect after surgery?
Immediately following the procedure, you may have some relief of pain from the numbing medication used during the procedure.
You will not be able to drive or do any physical activity for 24 hours.
You may experience an increase in pain for the first several days following the procedure. Additional pain medications may be necessary to make you comfortable. If these include narcotics, you will need to watch for constipation. Drink lots of fluids and eat foods with plenty of fiber. If constipation should occur you will need to use a laxative, available over-the-counter.
You may also note some swelling and bruising where the needle was inserted. Using a cold pack may ease the discomfort. Occasionally infection or bleeding can occur at the site of the procedure. If you have a fever of 101 degrees or greater, chills, or redness or drainage at the treatment site, call your doctor.
The degree of pain relief varies from person to person. The maximum decrease in pain may take up to three or more weeks to occur. You can eventually expect 50 percent or greater pain relief. Pain relief can last from six to12 months or even longer. The nerves do repair themselves and your pain may return. The procedure may be done again.
Your doctor will arrange a follow-up appointment, or phone consult within three to four weeks after the procedure to see how you are doing.
Rehabilitation
What should I expect during my rehabilitation?
It is important that you start a program of conditioning, strengthening, and range of motion exercises after radiofrequency ablation. Ideally, increased muscle strength around the arthritic joints will make them less painful for several months after radiofrequency ablation.