by admin | May 4, 2015 | Uncategorized
Anti-Inflammatory Diet Tips for Rheumatoid Arthritis:
Do restaurant meals and snack attacks leave you with rheumatoid arthritis aches and pains? Certain foods – some of your favorites, like steak and cookies – may be causing flareups. Find out what you should stay away from and how to pick tasty substitutes for a healthy rheumatoid arthritis diet…
When you have rheumatoid arthritis (RA), a restaurant menu or open refrigerator can seem like a test: Can you find foods that satisfy your cravings without making joints swell, ache and stiffen?
Definitely. It’s easier than you think. Read on…
You can still eat meat – as long as you choose leaner cuts. Crave salty snacks? Eat nuts instead of chips.
The key is following an anti-inflammatory diet, which helps you avoid RA flares. And these smarter food choices aren’t necessarily boring ones.
Antioxidant-rich fruits and vegetables, high-fiber grains and healthy fats all constitute a rheumatoid arthritis diet that can help you reduce RA aches – in a matter of days.“I start my RA patients on a general anti-inflammatory diet, and they feel better within a week,” says internist Leo Galland, M.D., whose book The Fat Resistance Diet (Three Rivers Press) is based on anti-inflammatory foods.
“Their pain and stiffness is greatly reduced.”
We asked RA experts how to avoid flareups without sacrificing your favorite treats. Here’s what they said:
1. Red meat, pork, poultry, eggs, butter
Why they’re RA triggers: These animal products contain harmful saturated fat, which increases inflammation in the body.
“After a single meal high in saturated fat, blood cells produce more inflammatory signals for several hours,” Dr. Galland says.
“Continue eating like that, and blood cells stay in this inflammatory state,” he adds.
For RA sufferers, that means joint and muscle pain, heartburn, fatigue and even acne.
Anti-inflammatory diet alternative: Love omelets? Whip one up with egg whites (the saturated fat is in the yolk).Proud of your milk mustache? Switch to skim. Can’t give up meat? Choose leaner cuts like sirloin steak, chicken breasts and pork loin chops.
If it’s protein you crave, get it from salmon or mackerel, which are rich in healthful omega-3 fatty acids (you’ll learn more about their health-boosting benefits in the next section).
But “get more fats from plant sources than animal,” says David Rakel, M.D, director of Integrative Medicine at the University of Wisconsin School of Medicine.
“Fat isn’t bad, but we need more polyunsaturated and monounsaturated fats, such as those found in olive oil, nuts and avocados.”
2. Store-bought chips, margarine
Why they’re RA triggers: These snacks and spreads contain trans-fatty acids (TFAs), oils that are chemically processed to make them more solid and stable.
A diet high in TFAs increases C-reactive protein, a marker doctors use to indicate the amount of inflammation in the blood, according to a 2004 Harvard Medical School study published in the American Journal of Clinical Nutrition.
The study showed that TFA-rich foods had a profound effect on inflammatory markers, making them twice as dangerous as saturated fats.“Adding TFAs to the American diet was one of the worst things we could have done. The body requires a lot more energy to break down trans fats, which creates inflammation,” Dr. Rakel says.
TFAs show up in many packaged and processed foods, but they’re easily detected: Just look at the nutrition label.
Since 2008, the Food and Drug Administration (FDA) has required that all U.S. food manufacturers list trans fats.
But watch out: Even if a label proclaims zero trans fats, it’s not necessarily free of them.
Federal regulations allow products containing up to half a gram of trans fat per serving to be labeled as “trans-fat free.”
That means consumers can easily exceed the maximum daily recommended amount of trans fats (1.11 grams) with just three pieces of toast spread with “trans-fat-free” margarine.A safer bet: Stay away from products that include partially hydrogenated oils on the ingredient list; that’s code for trans-fat content.
Anti-inflammatory diet alternative: Nuts and seeds contain omega-3 fatty acids, a healthier fat that reduces levels of C-reactive protein, according to a 2009 study published in the European Journal of Clinical Nutrition.
“When you crave a crunchy snack, dump the chips and scoop up a handful of walnuts, a great source of omega-3,” says Joan Levinthal, a registered dietitian in Woodland Hills, Calif.
Replace margarine with trans-fat-free spreads, such as Smart Balance Omega-3 Buttery Spread, which contains omega-3-rich flaxseed and fish oil.
3. Cakes, cookies, white bread, potatoes and white rice
Why they’re RA triggers: These comfort foods rank high on the glycemic index (GI).
They quickly break down into sugar, making insulin levels rise, which can cause inflammation.In fact, each 10-point increase in a diet’s glycemic status is associated with a 29% rise in C-reactive protein, according to a 2008 Netherlands study published in the Journal of Clinical Nutrition.
“Sugar increases the inflammatory [process],” says nurse practitioner Marcelle Pick, R.N.C., OB-GYN N.P., author of The Core Balance Diet (Hay House) and co-founder of Women to Women, a holistic medical clinic in Maine.
“If you must have something sugary, eat it with some protein to slow its breakdown into glucose.”
Anti-inflammatory diet alternative: By replacing white bread, potatoes and rice with moderate servings of whole-grain bread, sweet potatoes and brown rice, you’re eating on the lower end of the GI index.
Plus, you’re adding more fiber to your diet, which fights inflammation, according to the Arthritis Foundation.
Bing cherries have been found to reduce inflammatory markers, according to a 2006 study in The Journal of Nutrition.Apples and pears are also low on the glycemic scale. Baked and flavored with cinnamon, they’ll taste like a decadent dessert.
“Cinnamon has been shown to help regulate blood sugar; plus, it has a sweet taste all its own,” says registered dietitian Angela Ginn, a spokesperson for the American Dietetic Association.
4. Milk and wheat products
Why they’re RA triggers: Some foods trigger food-intolerance reactions, such as bloating, irritable bowel syndrome (IBS) and headaches.
If you have food sensitivities, your immune system creates antibodies every time you eat them, causing an inflammation cycle, according to Pick.
To prevent this, eliminate foods that disturb your gastrointestinal tract.
Anti-inflammatory diet alternative: Because intolerances differ by person, find out your food allergies first, then pick healthier substitutes.
In month one, Pick’s patients follow a strict month-long elimination diet that excludes common food triggers: sugar, dairy, wheat, eggs, citrus, caffeine, soy. They also keep track of physical reactions in a food diary.In month two, they slowly reintroduce missing foods, one at a time. Any foods that produce a negative reaction are permanently removed from the plate.
“After changing diets, some patients are able to go back to their doctors and ask to be taken off their RA medications,” Pick says.
By Barbara Stanifer, Lifescript

by admin | May 4, 2015 | Uncategorized
You finally sit down to relax at night after a long day at work, and bam! No sooner do you settle into that easy chair that a tightening sensation crawls up your legs, making you get up again. How can you rest when your legs are urging you to move? Here are tips to ease the symptoms of restless legs syndrome, so you can get the relaxation you need…
It feels like your legs constantly want to do the cha-cha, but the cause of restless legs syndrome (RLS) may not be in the lower limbs at all. It actually may be in the brain.
Scientists have found that low levels in the brain of a crucial chemical, dopamine, and a mineral, iron, may trigger the torturous twitching, tingling sensation that’s a hallmark of the disease affecting 10% of Americans.
“Anything that affects the body’s metabolism of dopamine will affect RLS symptoms,” says William Anderson, M.D., an internist who practices sleep medicine at the University of South Florida in Tampa.
That’s one reason scientists recommend therapies that target the brain to ease RLS symptoms, from raising levels of dopamine and iron to distracting the mind.
Here are some tricks you can try ease your symptoms, settle down and relax.
1. Raise levels of dopamine
“The problem is usually the dopamine level in the nerves,” says Lorne Label, M.D., chief of staff at Los Robles Hospital and Medical Center in Thousand Oaks, Calif., and clinical professor of neurology at University of California, Los Angeles.Increasing dopamine will help ease symptoms, he says.
Drugs containing “dopaminergic agents,” such as pramipexole and ropinirole, largely used to treat Parkinson’s disease, increase dopamine and have been shown to reduce symptoms of RLS, according to the National Institutes of Health.
“Folic acid also helps improve production of the neurotransmitter dopamine,” says Suzy Cohen, Lifescript pharmacist, R.Ph., and author of The 24-hour Pharmacist (William Morrow).
She recommends 800 micrograms (mcg) twice daily.
2. Check your iron
Low iron can be the main cause of RLS symptoms, Dr. Label says.
“If your ferritin [the protein that stores the body’s iron] level isn’t above 50 nanograms per milliliter, it’s not high enough,” Dr. Anderson says.
But the problem may not lie just with low iron levels but rather with how your brain processes it.Iron may be poorly absorbed in the brains of restless legs syndrome patients, according to 2003 Penn State University College of Medicine research that showed poor iron uptake in the brains of autopsied restless legs syndrome patients.
The “iron isn’t being delivered to certain brain cells in an effective way,” explains James R. Connor, Ph.D., who led the study.
To check whether you need iron supplements, see your doctor for a simple blood test.
3. Boost your B vitamin intake
“Folate [a B vitamin] increases blood flow (circulation) and, therefore, could improve RLS,” Cohen says.
Folic acid can be taken as supplements or through foods, such as peanuts, garbanzo beans, lentils and spinach in its naturally occurring form, folate.
Another B vitamin, B12, has also been directly linked to RLS, according to Dr. Anderson.
The recommended dietary allowance of vitamin B12 is 2.4 mcg. Ask your doctor if you might benefit from more.
4. Use a sequential compression device (SCD)
A sequential compression device is a mechanical sleeve that fits over the leg and massages it by inflating and deflating with air (much like the armband used to measure blood pressure). It’s usually used to prevent blood clotting in hospital patients, and one small study has shown it may help RLS patients too.
All nine patients who wore a sequential compression device (SCD) for one hour before bedtime every night for three months reported improved social and daily task function and quality of life, according to a 2007 study by the Department of Medicine at the Walter Reed Army Medical Center in Baltimore.
It might work because “the body is capable of only appreciating a limited number of stimuli simultaneously,” the Restless Legs Syndrome Foundation states, implying the sensory impact of the SCD won out over RLS.
5. Exercise
Working out may alleviate symptoms of restless legs syndrome, according to the National Institutes of Health. But don’t overdo it, cautions the RLS Foundation.
Mild exercise, such as walking, light jogging, or yoga, “may help RLS while vigorous exercise can trigger RLS symptoms in some individuals,” explains the RLS Foundation’s brochure, Triggers for Restless Legs Syndrome.
6. Adjust your medication
“Antipsychotics and antidepressants can worsen RLS,” says Winona Tse, assistant professor of neurology at Mount Sinai Medical Center in New York.
“They interfere with the body’s metabolism of dopamine.”
Any medication that blocks dopamine receptors, including anti-nausea drugs used to reduce vomiting, motion sickness and inner ear dizziness, can worsen symptoms of restless legs syndrome, according to the RLS Foundation. So can antihistamines, frequently used to treat colds and allergies.
If you experience an increase in RLS symptoms while taking other medications, see your doctor about alternatives, decreasing the dosage or possibly discontinuing the medication.
7. Don’t try melatonin
Though restless legs syndrome can disrupt sleep, this common over-the-counter sleep supplement won’t help, according to a 2004 Canadian study.
The naturally occurring hormone melatonin regulates your body’s internal clock, or circadian rhythms. Its levels typically increase at night and taper off toward daybreak.
Melatonin also inhibits the secretion of dopamine, which makes it bad news for restless legs syndrome patients. It might increase RLS symptoms in the evening and night, according to researchers at Sacre-Coeur Hospital in Montreal.
8. Take calcium and magnesium
Calcium and magnesium are minerals that aid in the functioning of muscles and nerves, so they may help RLS patients, Cohen says.
“If it’s low, then you definitely need to have your calcium and magnesium within the normal range,” Dr. Label says.
Cohen recommends a daily combination dose of 600 milligrams (mg) of calcium and 200 mg of magnesium.
“But if after 2-3 months there’s been no improvement, it’s not going to help,” Dr. Label warns.
9. Get a massage
Massaging legs before the onset of restless legs syndrome symptoms has been shown to be effective in a 2007 study published in the Journal of Bodywork and Movement Therapies.
It found that therapies such as deep tissue and sports massage for 45 minutes twice a week on the lower extremities reduced symptoms of RLS.
Symptoms were reported to decrease after two treatments and continued to improve over the following three weeks. 10. Run a warm bath (or cold shower)
“Taking a hot bath may relieve discomfort for a [short] time,” Dr. Label says.
However, once you get out of the bath, the symptoms will probably return, he says.
“Others say a cold shower is soothing,” says the RLS Foundation. “Ice packs and heating pads have also been used for relief.”
Whether hot or cold temperatures work depends on the individual, it says.
Other Coping Techniques
The foundation suggests other methods for coping with symptoms of restless legs syndrome in various situations. They include:
- Working the nightshift. Because RLS is tied to the body’s circadian rhythms and worsens at night, it may help to work during the wee hours. By staying active at night, there may be relief during the day.However, check with your health-care provider before changing your schedule: There may be other health consequences to staying up all night, the RLS Foundation says.
- Traveling in the morning. Because sitting still for long periods can be challenging for those with restless legs syndrome, plan a long car ride and air travel for the morning hours. This is especially key for overseas flights or trips that involve a change in time zone, factors that further complicate your body’s natural rhythms.
- Requesting a standing work station. Many variations are available to the standard desk. Many people now work standing, at a podium-like work station. This not only may help RLS, but it also improves circulation throughout the body.
- Staying engaged. Bringing snacks to work or on long trips can distract the mind from the onset of RLS symptoms. For example, eating one popcorn kernel or raisin at a time may be enough. Also be sure to pack enough activities and reading material to stay absorbed during a long trip.
- Quitting caffeine. Although no formal research exists that shows a reduction in caffeine intake can lessen the symptoms of RLS, several patients have reported that quitting the stimulant has helped.
“Caffeine has been linked to an increase in RLS symptoms,” the Restless Legs Syndrome Foundation states. “[It] is present in coffee, tea, chocolate, soda, and other common foods and beverages. Check ingredient listing carefully.”
By Sally Schultheiss, Lifescript

by admin | May 4, 2015 | Uncategorized
What would you do if rheumatoid arthritis ended a thriving life as a star cake artist? Catherine Ruehle, a former contestant on “Food Network Challenge,” faced that situation. In this exclusive interview, she shares how her anti-inflammatory RA diet and lifestyle led to a new career…
Catherine Ruehle, 45, was known for creating one-of-a-kind cake masterpieces at her Sublime Bakery in Fort Worth, Texas.
So when the seasoned baker appeared on the reality show “Food Network Challenge” in 2010, her competitors were ready for a formidable opponent.
But Ruehle surprised everyone – including herself – when she had to withdraw from the show. The reason? Her hands stopped working as she was making a cake.
At first, she chalked up her symptoms to long hours in the bakery. But when her hand pain worsened, she saw a doctor. The diagnosis: rheumatoid arthritis (RA), a chronic autoimmune disease that causes joints to become inflamed and painful.
“I was shocked,” Ruehle tells Lifescript. “I was 41 at the time, and always believed RA was an elderly person’s disease.”
In fact, RA most commonly begins between ages 30 and 60 but can occur even earlier, according to the Arthritis Foundation. Its symptoms can build slowly or strike suddenly, as it did with Ruehle.
Still, she couldn’t just stop baking, so she “plodded along in denial,” she says.
“When I first started experiencing pain in my hands, it was Christmas – the busiest season at my bakery – and I couldn’t take time off,” Reuhle says. “It became hard to do everyday tasks, such as [screwing] the top off a water bottle or bending my elbows to brush my hair.”
Finally, she had to close her bakery in 2011. But Reuhle’s food career wasn’t over. She now has a business helping other people improve their health with diet and lifestyle changes.In this exclusive Lifescript interview, Ruehle reveals how she has learned to manage her condition through an anti-RA diet.
What symptoms led to your RA diagnosis?
I had pain and stiffness throughout my entire body – it started in my hands and spread to my elbows, ankles, legs and toes. The pain was so bad that I initially worried I might have bone cancer.
Is that what led you to see a doctor?
I procrastinated when it came to making a doctor’s appointment. It was the holiday season and I was swamped. I convinced myself that my body was just tired from spending long hours in the bakery.
What convinced you to see a doctor?
The [symptoms got worse, so] I went to see my doctor. I asked if there was a way to alleviate my pain so that I could enjoy Christmas with my family, and then return for testing.
He gave me a shot of prednisone [an anti-inflammatory steroid], which immediately eased my stiffness.
After the holidays, I went in for tests, which included blood work and a rheumatoid factor blood test. The tests indicated that I had RA.
[Editor’s note: No single test can confirm RA, so Ruehle’s doctor asked about her joint symptoms, how and when they started, how severe they were, and what, if anything, made them better or worse. She was also given a blood test that measured her inflammation levels and the rheumatoid factor blood test, which measures the antibody most common in RA. Although high levels of rheumatoid factor are associated with more severe rheumatoid disease, it can also be present in patients with other conditions such as lupus or hepatitus and in people who have family members with RA.]
What was your reaction to the RA diagnosis?
While I was glad I didn’t have bone cancer, I was shocked to learn I had RA. I lead an active lifestyle, and have always eaten healthfully – I felt as if my body was betraying me.
I also didn’t [know] how severely it would affect my life. I wondered if I would eventually have disfigured, arthritic hands.
I immediately began to read everything I could find out about RA so that I could weigh my treatment options.
What did you learn about the condition?
I was intrigued by evidence that RA is caused by an overactive immune system. I realized my immune system was angry and attacking my body.
I wanted to see if I could treat the cause with anti-RA diet and lifestyle changes. I discovered a functional medicine expert, Dr. Mark Hyman, and adopted his mantra as my own: “Treat the fire, not the smoke.”
How did your rheumatologist feel about this idea?
[He] told me diet had nothing to do with RA inflammation. But my gut told me that [what I ate] would have everything to do with my long-term health.
What dietary changes have you made?
I [now] describe my diet as a whole foods, mostly organic plan that’s also free of corn, gluten and dairy.
I discovered evidence that foods, such as vegetables and omega-3 [oils in] fish, can ease an overactive immune system. And I decided to load up on nutrient-dense plant foods and drink green juice daily.But I avoid nightshade vegetables (such as tomatoes, peppers and eggplants), because I found they set off my arthritis symptoms.
[Editor’s note: Some arthritis patients say these vegetables increase symptom flares; there’s little scientific proof that they cause inflammation].
While I enjoyed a couple glasses of wine for my recent birthday, I can’t drink it every night because it also exacerbates my condition.
With your anti-RA diet, was it hard to give up certain foods?
I’m a foodie, so it wasn’t easy. Rather than concentrate on foods I couldn’t have, I tried to focus on what I could eat.
What are some of your favorite healthy foods?
[In place of] cow’s milk, I now use coconut milk for cooking and in smoothies. It contains selenium, an important antioxidant that controls free radicals and has been shown to relieve the symptoms of arthritis.
[Editor’s note: Selenium-rich foods, which also include whole grains and shellfish, may be useful in preventing arthritis symptoms, according to the Arthritis Foundation.]
I also eat a lot of green, leafy vegetables. I had never eaten kale before [my diagnosis]; now I have it every day. I also eat hemp seeds, nuts such as walnuts and almonds, and cold-water fish including salmon and sardines – all inflammation-fighting foods.
What other lifestyle changes have you made?
I’ve started working to eliminate stress in my life, which has shown to be a cause of RA flare-ups.How do you combat stress?
I’ve become addicted to yoga and subscribe to an online service that streams yoga videos. I’ve found that practicing it daily not only strengthens the core and improves flexibility, it also helps me sleep better, feel more centered and clear-headed, and gives me more energy.
I went through a divorce this past year and lost my father, and I know doing yoga helped me cope better with the loss and stress.
Are you still working as a chef?
I closed my bakery shortly after my diagnosis, because [the business] involved long, unpredictable hours. I needed a schedule that was more manageable and less stressful.
How did your RA diagnosis lead to a career change?
In my quest to learn more about the effects of diet on health, I enrolled in a yearlong online study program through the Institute for Integrative Nutrition, where classes are taught by health experts, including Dr. Andrew Weil and Dr. Deepak Chopra.
I have a business, A Well-Nourished Life, where I create individualized wellness programs, including meal plans. My goal is to help [people with chronic illnesses] improve their symptoms and regain their health. I do custom meal planning and preparation for some clients.
And I just finished writing Gluten Free Cakes, a cookbook that will be published by Ten Speed Press [in September 2014].
Have you found any gadgets that make cooking easier?
One of my favorite tricks is using those nonstick squares that you place under rugs to open bottles. They make it so much easier! Oxo also makes a vegetable peeler with oversized rubber handles.
I also use a gel floor mat in the kitchen that can make it easier on your knees if you’re standing and cooking for long periods of time.
How’s your health today?
I’m doing great and continue to be primarily pain- and symptom-free – as long as I stick to my diet and exercise regimen.Here are three of Ruehle’s anti-RA recipes.
All recipes reprinted with permission from Catherine Ruehle’s A Well-Nourished Life.
Oven Roasted Beets & Brussels Over Kale with Raw Honey-Ginger Dressing
Serves: 2-4
Ingredients
2 medium beets, washed, peeled and cubed
3 cups whole Brussels sprouts, washed & halved
1 tablespoon extra virgin olive oil
1 head kale, washed and coarsely chopped
Pinch pink Himalayan sea salt (optional)
2 tablespoons pine nuts (optional)
1 tablespoon fresh ginger root, grated
1 tablespoon raw honey
1 lemon, juice only
1-2 teaspoons organic oil, such as toasted sesame or extra virgin olive oil
Salt & pepper to taste
Preparation
1. Preheat oven to 400 degrees.
2. Toss the beets and Brussels sprouts with the olive oil in a bowl to coat well. Spread out on a foil-lined baking sheet in a single layer.
3. Roast in the oven until tender and darkened at the edges, about 25 minutes, rotating the pan halfway through the cooking time.
4. While the veggies are roasting, combine the dressing ingredients in a small bowl and whisk together.
5. Toss the chopped kale with half the dressing and set aside while veggies roast.
6. Remove veggies from oven. Spread the kale on the serving plates. Place the hot veggies in the same bowl the kale was in and add the remaining dressing; toss to coat.
7. Layer the beets and Brussels sprouts over the kale on the serving plates. Top with the sea salt and pine nuts. Season with salt and pepper to taste.Zucchini & Herb Fritters with Mint-Yogurt Sauce
Ingredients
3 large zucchini, grated
1 teaspoon salt
1 shallot, diced
1 garlic clove, diced
2 eggs
1 tablespoon chopped fresh mint
1/2 cup crumbled feta cheese (optional)
1/4 cup gluten-free flour mix (I like Angel’s), or all-purpose flour if not gluten-free
Salt & pepper to taste
Olive oil for sautéing
For the Yogurt-Mint Sauce:
1 cup Greek yogurt (or nondairy yogurt like Amonde or So Delicious)
2 tablespoons chopped fresh mint
1 tablespoon chopped fresh dill
Juice of 1 lemon
Salt and pepper to taste
Preparation
1. Place the grated zucchini in a colander and sprinkle with the salt. Allow to sit for about 15 minutes while you chop your shallot and garlic.
2. Squeeze the excess moisture out of the zucchini then place in a large bowl.
3. Add shallot, garlic, eggs, mint, feta and flour to the zucchini. Combine and season with salt and pepper.
4. Add enough olive oil to your saute pan to coat the bottom of the pan and heat over medium. While pan heats, use your hands, two spoons, or an ice cream scoop, to form balls of zucchini mixture.
5. Place 3-4 balls into your hot pan, and press down to flatten to about 1 inch tall. Make sure you keep at least 2 inches between each fritter so they will brown nicely and not “steam” each other.
6. Cook on each side for about 2-3 minutes until golden. Remove to a paper towel to drain.
7. Combine all ingredients for the Yogurt-Mint Sauce.
8. Serve fritters warm or room temperature with sauce on top or on the side.
Note: Fritters will keep in the refrigerator for 3 days or in the freezer for 1 month. Sauce keeps in refrigerator for 3 days. Vegan Chocolate Pudding
Serves: 4
Ingredients
2 ripe avocados, peeled and pit removed
1 cup canned coconut milk, chilled overnight and liquid drained off
3/4 cup organic maple syrup
3/4 cup raw organic cacao powder
1 teaspoon pure vanilla extract
1 teaspoon ground cinnamon
Pinch fine sea salt
Preparation
1. Add all ingredients to a blender or food processor and blend until smooth.
Note: you want to use only the thick coconut “cream,” reserve the liquidy coconut water for another use such as smoothie. Don’t skip the chilling step or you may not be able to separate the cream from the water, resulting in a thin pudding.

by admin | Apr 30, 2015 | Uncategorized
Weekly Breaking Research Updates
Scientific breakthroughs happen every day! In an effort to help our patients stay up to speed on the most cutting edge treatment options available for them, our scientists monitor current research and publish weekly research updates. The title of each article below is a link to the full study report. If you’d like to make an appointment with Dr. Hanna to discuss your treatment options, please contact us.
Ketamine
Rapid antidepressant Action and Restoration of Excitatory Synaptic Strength after Chronic Stress by Negative Modulators of alpha5-containing GABAA Receptors.
J Fischell, AM Van Dyke, MD Kvarta, TA LeGates… – … : official publication of the …, 2015
… The NMDA receptor antagonist ketamine exerts a rapid antidepressant action, but
has troubling side-effects. We hypothesized that negative allosteric modulators of
GABAA receptors would exert similar effects on brain activity …
Temporal evoltion on MRI of successful treatment of rabies
A Lu, P Shah, P Shen, P Lee, AE Nidecker… – Clinical Imaging, 2015
… Her treatment regimen came to be known as the “Milwaukee protocol” [1]. Briefly, the
protocol consists of using a sedative agent such as ketamine, midazolam, propofol, or
a combination to place the patient in a medically induced coma. …
[PDF] A Gelatin-Based Prophylactic Sealant for Bowel Wall Closure, Initial Evaluation in Mid-rectal Anastomosis in a Large Animal Model
Y Kopelman, Y Nir, Y Siman-Tov, B Person, O Zmora – J Gastrointest Dig Syst, 2015
… Preemptive analgesia (intramuscular Dipyron 1 gr) was given to all any amounts prior to surgery.
The animals were anesthetized with a combination of Ketamine 22 mg/mL and Xylazine injection
(Apectrum Chemicals and Laboratory Products, Gardena, California) 1 mg/kg IM. …
[PDF] The optimal fitting model for aging-related receptive field size curve of macaque V1 neurons
J Cui, H Ding, L Wang, J Qiang – … on Mechatronics, Electronic, Industrial and Control …, 2015
… of 28 years. An initial ophthalmological examination was performed under ketamine
(100 mg/kg im, Ketalar, Parke-Davis, Morris Plains, NJ, USA) anesthesia to screen
for monkeys with ocular pathology. B. Visual Stimulation …
[PDF] Preventing Testicular Damage in Genital Burns With Cooling: An Experimental Study
AE Abalı, H Özdemir
… The sham group (S group) consisted of 10 healthy testes. In this group, rats were anesthetized
with an intraperitoneal injection of 100 mg/kg ketamine hydrochloride (Alfamine 10%, Alfasan,
Holland) and 10 mg/kg … Animals were killed by high-dose ketamine HCl. …
[PDF] JAMES A. McNAMARA, JR., DDS, Ph. DT
T KURODA
… Page 2. Ketamine & Phencyclidine . . . … Dosage, prepared according to levels
recommended by other investigators-fit10:11 was as fol- lows: phencyclidine HCl,
1.5 ngkg. of body weight (intramuscular); ketamine HCI, 25 mgjkg. …
Fine-scale genetic structure of the ringtail (Bassariscus astutus) in a Sky Island mountain range
RC Lonsinger, RM Schweizer, JP Pollinger, RK Wayne… – Journal of Mammalogy, 2015
… Traps were baited with dry cat food and either loganberry paste or sardines. Captured ringtails
were anesthetized using a mixture of medetomidine hydrochloride (50 µg/kg) and ketamine
hydrochloride (5mg/kg) injected intramuscularly (Orion Corporation, Espoo, Finland). …
[PDF] Evaluation of the Effect of Alfalfa Extract on Breast Cancer
F Nabatchian, SMH Aghoosi, A Mordadi, F Khodaverdi – J. Appl. Environ. Biol. Sci, 2015
… normal saline. In the solution, the tumor was cut into 3 mm2 pieces. Then, the mice
in the first and second groups were anesthetized with intraperitoneal injection of
ketamine (10 mg/kg) and xylene (5 mg/kg). The tumor pieces …
Effects of light pollution on seasonal estrus and daily rhythms in a nocturnal primate
T LeTallec, M Théry, M Perret – Journal of Mammalogy, 2015
… Ltd, Saint-Paul, Minnesota) previously implanted in the visceral cavity under general anesthesia
and under veterinary supervision (Diazepam-Valium: 1mg/100g, subcutaneous injection; Ketamine
hydrochloride-Imalgen: 10mg/100g, intraperitoneal injection; postoperative …
[PDF] Evaluation of Cissampelos pareira root for antifertility activity
J Samanta, S Bhattacharya, AC Rana – Journal of Pharmacy Research Vol, 2015
… from D1 pregnancy. On day 12th day (D12) all the rats of control and treated group
were anaesthetized with normal dose of ketamine-xylazine anaesthesia15 and
laparotomized to count the no. of implants of each rat. 2.3.6. Effectsof …
Radiofrequency Ablation (RFA)
[HTML] Transcatheter embolization therapy in liver cancer: an update of clinical evidences
YXJ Wáng, T De Baere, JM Idée, S Ballet – Chinese Journal of Cancer Research, 2015
… 2-4). For the treatment of early stage HCC, curative therapies including liver transplantation,
hepatic resection, and radiofrequency ablation (RFA) are … coagulative necrosis of both the tumor
and a rim of surrounding parenchymal tissue producing a margin of ablated non-tumoral …
CATHETER WITH ATRAUMATIC TIP
ES Olson, JV Kauphusman, LK Nemec, TT Tegg – US Patent 20,150,112,331, 2015
… According to at least one medical study (See, eg, Ikeda et al., Radiofrequency Ablation Catheter
with Contact Force Sensor Predicts Lesion Size and Incidence of Steam Pop in the Beating Canine
Heart, Conference Proceedings of the Hearth Rhythm Society, May 2008 and …
ELECTRICAL STIMULATION OF THE CAROTID ARTERY
I Gillbe – US Patent 20,150,112,359, 2015
… or bodies without heating the tissues to a temperature at which they are ablated such that … the
RF energy delivered is of a non-thermal nature, so that ablation and possible … As previously
described, pulsed radiofrequency is employed for this purpose; comprising short bursts of …
METHOD TO REDUCE SENSE OF TASTE AND FOOD INTAKE
H Li – US Patent 20,150,112,326, 2015
… To ablate the subsurface tissue without ablating the surface tissue of the mouth, a room … During
a heat induced ablation with fluid cooling, ablation head and the tissue surface in … delivered into
it from an energy source such as ultrasound, microwave, and radiofrequency current. …
MODULATION OF NERVES INNERVATING THE LIVER
BR Azamian, JA Coe, SB Vafai – US Patent 20,150,112,332, 2015
… In some embodiments, the neuromodulation catheter is a radiofrequency (RF) ablation catheter
comprising … about substantially 180 degrees of the vessel circumference to ablate in a … In some
embodiments, other patterns of ablation electrode movement (regardless of inherent …
BALLOON CATHETERS WITH FLEXIBLE CONDUCTING WIRES AND RELATED METHODS OF USE AND MANUFACTURE
MR Willard, DC Sutermeister, KR Larson, TA Ostroot… – US Patent 20,150,112,328, 2015
… Sympathetic nerve ablation device 12 may be used to ablate nerves (eg, renal nerves) disposed
adjacent to the kidney K (eg, renal nerves … Sympathetic nerve modulation device 12 may be
configured to deliver ablation energy, for example, radiofrequency energy, to a target …
Current Control Methods and Systems
H Cadouri – US Patent 20,150,112,321, 2015
… an energy field to a target site in the renal artery (eg, via radiofrequency ablation) have been … above
45° C. (or above 60° C. in other cases) may induce thermal ablation of the … In some patients, it
may be desirable to achieve temperatures that thermally ablate the target neural …
DIAPHRAGM ENTRY FOR POSTERIOR SURGICAL ACCESS
SD Fleischman, R Neubert, EW Rogers – US Patent 20,150,112,145, 2015
… Atrial fibrillation surgery involving radiofrequency, DC, microwave, ultrasound, laser or other
modes of thermal … of focusing energy into local areas spaced at known distances from the ablation
device (in … tissue in the ventricles from the diaphragm) are used to ablate the imaged …
[PDF] ASRA/ESRA/INS/AAPM/WIP/NANS guidelines for interventional spine and pain procedures in patients on antiplatelets and anticoagulants
S Narouze, HT Benzon, D Provenzano, A Buvanendran…
… C, cervical; T, thoracic; L, lumbar; S, sacral; MBNB, medial branch nerve block; RFA,
radiofrequency ablation *Patients with high risk for bleeding undergoing low or intermediate
risk procedures should be treated as internmediate or high risk repectively. …
SYSTEM AND METHOD FOR TREATING URINARY TRACT DISORDERS
U Eshel – US Patent 20,150,112,413, 2015
… transurethral microwave thermotherapy (temperatures over 46 degrees Celsius that cause tissue
ablation to exposed … that the higher level of heat in the surrounding non-ablated tissue either … It
includes a catheter with a sheathed radiofrequency antenna, surrounded by a flow of …
Complex Regional Pain Syndrome (CRPS/RSD)
What is the maximum safe tourniquet time in elective upper limb surgery?
N Sawant, GEB Giddins – Journal of Hand Surgery (European Volume), 2015
… Two patients developed chronic regional pain syndrome type 1 (CRPS 1). In one patient this
was noticed 4 weeks following complex rheumatoid surgery. The tourniquet time was 2 hours
4 minutes and there was no immediate post-operative pain or distal paraesthesia. …
RODENT RUN
MJ Dixon, PM Taylor, B Dixon – US Patent 20,150,107,525, 2015
… [2] Millecamps, Laferrière, Ragavendran, Stone, Coderre: “Role of peripheral endothelin receptors
in an animal model of complex regional pain syndrome type 1 (CRPS-I)” J Pain, volume 151
(2010) pages 174-183; [3] Ugo Basile Leaflet for Von Frey Hairs (with grid) Cat. No. …
Using Computing with Words for Managing Non-cooperative Behaviors in Large Scale Group Decision Making
FJ Quesada, I Palomares, L Martínez – Granular Computing and Decision-Making, 2015
… sufficiently to reach the solution made. In order to overcome this drawback, Consensus
Reaching Processes (CRPs) were introduced as an additional phase in the resolution
process for GDM problems [17]. In a CRP, experts try …
The Parturient With Implanted Spinal Cord Stimulator: Management and Review of the Literature
AC Young, TR Lubenow, A Buvanendran – Regional Anesthesia and Pain Medicine, 2015
… Complex regional pain syndrome (CRPS) is neuropathic pain syndrome that is more common
in women, with some studies showing a higher prevalence among women aged 25 to 50
years. … Patient 3 suffered from CRPS of the right upper extremity. …
Decision Makers’ Opinions Changing Attitude-Driven Consensus Model under Linguistic Environment and Its Application in Dynamic MAGDM Problems
B Dutta, D Guha – Granular Computing and Decision-Making, 2015
… Based on the concept of soft consensus, vari- ous consensus reaching processes
(CRPs) have been designed in the literature [22]. The existing CRPs for solving GDM
problems can be classified in two categories: static consensus …
Peripheral Nerve Stimulationperipheral nerve stimulation
AS Hanna – Anatomy and Exposures of Spinal Nerves, 2015
… Download Chapter (482 KB). Abstract. Peripheral nerve stimulation is an off-label use of spinal
cord stimulators. It is used for intractable pain in a peripheral nerve distribution, refractory to
medical management, especially with complex regional pain syndrome (CRPS ). …
[HTML] External Fixation and Adjuvant Pins Versus Volar Locking Plate Fixation in Unstable Distal Radius Fractures: A Randomized, Controlled Study With a 5-Year Follow- …
JH Williksen, T Husby, JC Hellund, HD Kvernmo… – The Journal of Hand …, 2015
… At the 5-year follow-up, 3 patients had died, 1 (with an extensor pollicis longus rupture) had moved
abroad, and 2 (1 patient with complex regional pain syndrome [CRPS]) withdrew from the study. …
Carpal tunnel syndrome, 2, 1. CRPS, 0, 1. Extensor tendon synovitis, 0, 5. …
Complex regional pain syndrome type I: a comprehensive review
M Bussa, D Guttilla, M Lucia, A Mascaro, S Rinaldi – Acta Anaesthesiologica …, 2015
… Background. Complex regional pain syndrome type I (CRPS I), formerly known as reflex
sympathetic dystrophy (RSD), is a chronic painful disorder that usually develops after a
minor injury to a limb. … Pathophysiological mechanisms of CRPS I. …
Phenotype-Specific Diagnosis of Functional (Psychogenic) Movement Disorders
AJ Espay, AE Lang – Current Neurology and Neuroscience Reports, 2015
Page 1. MOVEMENT DISORDERS (M OKUN, SECTION EDITOR) Phenotype-Specific
Diagnosis of Functional (Psychogenic) Movement Disorders Alberto J. Espay1,3 & Anthony
E. Lang2 © Springer Science+Business Media New York 2015 …
[PDF] Time-consistent calibration of short-term regional wind power ensemble forecasts
S SPäTH, L VON BREMEN, C JUNk, D HEINEMANN – 2015
… For minimum score esti- mation, we use the continuous ranked probability score (crps). … For
a forecast cumulative distribution function (cdf) Fp(x) and the verifying obser- vation y, the crps
can be calculated as: crps(Fp,y) = ∞ ∫ − Fp(x) − Θ(x − y) ]2 dx (4.4) …
Efficient production of a correctly folded mouse α-defensin, cryptdin-4, by refolding during inclusion body solubilization
S Tomisawa, Y Sato, M Kamiya, Y Kumaki, T Kikukawa… – Protein Expression and …, 2015
… The mouse Paneth cell α-defensins, termed cryptdins (Crps) 1 , are secreted into the lumen of
the small intestinal crypts in response to exposure to bacteria or bacterial antigens [6]. Among
the known isoforms, cryptdin-4 (Crp4) has the most potent antimicrobial activity [7 …
[PDF] Erythrocyte Sedimentation Rate, C-Reactive Protein and Procalcitonin in Infections of the Spine and Infections in Spinal Cord Injury Patients
JAL Buensalido, MP Reyes – Open Infectious Diseases Journal, 2015
… One study reported a mean CRP of 3 mg/L in paraplegics, while a mixed paraplegia/tetraplegia
study that excluded patients with CRPs >10 mg/L, also showed a mean of 3 mg/L. Another group
noted that mean CRP level was 38 mg/L, or 27% higher, in SCI versus non-SCI …
Fibromyalgia
The role of sleep in pain and fibromyalgia.
EH Choy – Nature reviews. Rheumatology, 2015
Fibromyalgia is a common cause of chronic widespread pain, characterized by reduced
pressure pain thresholds with hyperalgesia and allodynia. In addition to pain, common
symptoms include nonrestorative sleep, fatigue, cognitive dysfunction, stiffness and mood …
Nonpharmacological Treatments of Insomnia for Long-Term Painful Conditions: A Systematic Review and Meta-analysis of Patient-Reported Outcomes in …
NK Tang, ST Lereya, H Boulton, MA Miller, D Wolke… – Sleep, 2015
… This study evaluated the effect of nonpharmacological sleep treatments on
patient-reported sleep quality, pain, and well-being in people with long-term cancer
and non-cancer (eg, back pain, arthritis, fibromyalgia) pain conditions. …
COMPOSITIONS AND METHODS FOR TREATING INTESTINAL HYPERPERMEABILITY
S Hoffman – US Patent 20,150,111,878, 2015
… Abstract: The present invention provides methods, compositions, and kits for treating intestinal
hyperpermeability in a subject in need thereof, including underlying diseases such as diabetes,
autism, fibromyalgia, inflammatory bowel disease (IBD), graft versus host disease …
American College of Lifestyle Medicine Expert Panel Discussion Treat the Cause: Evidence-Based Practice*
JM Rippe, M Greger, DL Katz, JH Kelly, M Moore… – American Journal of …, 2015
… Following this strategy, I am fostering clinical evaluation of coaching for fibromyalgia,
for which there is no good treatment other than exercise. However, it has taken 10
years to get to the place where we have enough coaches …
Whole body vibration training in patients with COPD A systematic review
R Gloeckl, I Heinzelmann, K Kenn – Chronic Respiratory Disease, 2015
… Abstract. In recent years, several studies have shown that whole body vibration training (WBVT)
may be a beneficial training mode in a variety of chronic diseases and conditions such as
osteoporosis, fibromyalgia, multiple sclerosis, or chronic low back pain. …
[PDF] Fibromyalgia Syndrome AmongIraqi Patients with Systemic Lupus Erythematosus: A Case Control Study
ZS Al-Rawi, HAJ Badran, FI Gorial
Abstract: Objective: To determine the prevalence of fibromyalgia syndrome (FMS) among
Iraqi patients with systemic lupus erythematosus (SLE) and its association with disease
activity. Patients and methods: This case control study included 100 patients with SLE and …
[PDF] Quality of life, sense of coherence and experiences with three different treatments in patients with psychological distress in primary care: a mixed-methods study
T Arvidsdotter, C Taft, B Marklund, S Kylén – BMC Complementary and Alternative …, 2015
… More detailed data on the procedure are reported elsewhere [48]. The patients had a primary
diagnosis of depression, anxiety or panic disorders, severe stress, somatic symptoms/pain
(including irritable bowel syndrome, fibromyalgia, migraine, fatigue) or sleep disorders. …
SULFUR-CONTAINING BICYCLIC COMPOUND
N Shiraishi, H Hoshii, W Hamaguchi, E Honjo… – US Patent 20,150,111,876, 2015
… containing bicyclic compound having a PAM action of GABA B , and it use for preventing
and/or treating schizophrenia, CIAS, cognitive impairment, fragile X syndrome, autism spectrum
disorder, spasticity, anxiety disorder, substance addiction, pain, fibromyalgia, or Charcot …
TOPICAL REGIONAL NEURO-AFFECTIVE THERAPY
R Aung-din – US Patent 20,150,111,930, 2015
… respective receptors. They are indicated for such diverse and seemingly different
conditions as: focal onset seizures, post-herpetic neuralgia, diabetic peripheral
neuropathy, fibromyalgia, anxiety, and drug withdrawal syndromes. The …
Associations between the functional CD40 rs4810485 G/T polymorphism and susceptibility to rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis
YH Lee, SC Bae, SJ Choi, JD Ji, GG Song – Lupus, 2015
[HTML] Response to Vitamin B12 and Folic Acid in Myalgic Encephalomyelitis and Fibromyalgia
B Regland, S Forsmark, L Halaouate, M Matousek… – 2015
Background Patients with myalgic encephalomyelitis (ME, also called chronic fatigue
syndrome) may respond most favorably to frequent vitamin B12 injections, in vital
combination with oral folic acid. However, there is no established algorithm for …
Cardiovascular control in women with fibromyalgia syndrome: do casual methods provide non redundant information compared to more traditional approaches?
AR Zamunér, A Porta, CP Andrade, A Marchi, M Forti… – American Journal of …, 2015
Abstract The cardiovascular autonomic control and the baroreflex sensitivity (BRS) have
been widely studied in FMS patients through the computation of linear indices of
spontaneous heart period (HP) and systolic arterial pressure (SAP) variabilities. However, …
Aberrant Analgesic Response to Medial Branch Blocks in Patients With Characteristics of Fibromyalgia
CM Brummett, AG Lohse, A Tsodikov, SE Moser… – Regional Anesthesia and …, 2015
Abstract Background and Objectives: Facet interventions for spine pain have high failure
rates, and preprocedural prediction of response is nearly impossible. A potential explanation
may be aberrant central pain processing as that existing in conditions like fibromyalgia. To …
[HTML] Effects of Whole-Body Vibration Therapy in Patients with Fibromyalgia: A Systematic Literature Review
D Collado-Mateo, JC Adsuar, PR Olivares… – … -Based Complementary and …, 2015
Objective. To review the literature on the effects of whole-body vibration therapy in patients
with fibromyalgia. Design. Systematic literature review. Patients. Patients with fibromyalgia.
Methods. An electronic search of the literature in four medical databases was performed to …
Six Syndromes with Surprising Psychotherapy Solutions
T Rodriguez, V Stern – Scientific American Mind, 2015
… These links to content published by NPG are automatically generated. Cognitive behavioral
therapy for fibromyalgia. … Utility of cognitive behavioral therapy as a treatment for insomnia in
patients with fibromyalgia. Nature Clinical Practice Rheumatology (01 Apr 2006). …
Comorbid Conditions Do Not Differ in Children and Young Adults with Functional Disorders with or without Postural Tachycardia Syndrome
G Chelimsky, K Kovacic, M Nugent, A Mueller… – The Journal of Pediatrics, 2015
… All patients underwent formal autonomic testing, Beighton scores assessment for joint
hypermobility (0-9), and fibromyalgia tender points (0-18) (43 subjects). Results. … All subjects with
fibromyalgia by tender point-examination had a Beighton score ≥4 (P = .002). Conclusions. …
Mast cell infiltrates in vulvodynia represent secondary and idiopathic mast cell hyperplasias
S Regauer, B Eberz, C Beham‐Schmid – APMIS, 2015
… Similar to other chronic pain syndromes among which are chronic pelvic and bladder pain,
fibromyalgia, and atopic dermatitis morphological correlates are hyperinnervation and increased
infiltrates of mast cells [3-5]. Activated mast cells release pre-stored or rapidly produced …
Biological stress systems, adverse life events and the onset of chronic multisite musculoskeletal pain: a 6-year cohort study
E Generaal, N Vogelzangs, GJ Macfarlane, R Geenen… – Annals of the Rheumatic …, 2015
… Previous studies mostly defined chronic widespread pain, a cardinal symptom of the fibromyalgia
syndrome, as axial and bilateral pain above and below the waist.41 With this somewhat ‘less
stringent’ definition, we may have included some patients with milder pain. …
Speed, science and optimal pain relief
RA Moore – International Journal of Clinical Practice, 2015
… For example, a retrospective analysis of patients with chronic back pain or fibromyalgia revealed
that patients rated their treatment as successful if their pain was reduced by 50–70%, from a level
of 5–10 on a visual analogue scale (total score 10) to below three (no more than …
[PDF] An Insight of D 鄄 Ribose Metabolic Imbalance in Type 2 Diabetes Mellitus
T SU, RQ HE – Progress in Biochemistry and Biophysics, 2015
… 14-15]. Ribose is often marked as a supplement for bodybuilders with a common
recommended daily dose of 5g or more and has also been used to reduce fatigue
in fibromyalgia and chronic fatigue syndrome [2,16]. Ribose …

by admin | Apr 28, 2015 | Uncategorized
Fibromyalgia Syndrome: Your Questions Answered
Fibromyalgia syndrome is a common and chronic disorder characterized by widespread pain, diffuse tenderness and many other symptoms. So what do sufferers really need to know? Find out now…
Although fibromyalgia is often considered an arthritis-related condition, it’s not truly a form of arthritis (a disease of the joints) because it doesn’t cause inflammation or damage to the joints, muscles or other tissues.
But like arthritis, fibromyalgia can cause significant pain and fatigue that can interfere with a person’s daily activities. Also like arthritis, fibromyalgia is considered rheumatic, a medical condition that impairs the joints and/or soft tissues and causes chronic pain.
People with fibromyalgia may experience a variety of other symptoms, including:
- Cognitive and memory problems (sometimes referred to as “fibro fog”)
- Sleep disturbances
- Morning stiffness
- Headaches
- Irritable bowel syndrome
- Painful menstrual periods
- Numbness or tingling of the extremities
- Restless legs syndrome
- Temperature sensitivity
- Sensitivity to loud noises or bright lights
Fibromyalgia isn’t a disease, but a syndrome: a collection of signs, symptoms and medical problems that tend to occur together but are not related to a specific, identifiable cause. A disease, on the other hand, has a specific cause or causes and recognizable signs and symptoms.
Who Gets Fibromyalgia?
Scientists estimate that fibromyalgia affects 5 million Americans age 18 or older. For unknown reasons, between 80% and 90% are women; however, men and children also can be affected. Most people are diagnosed during middle age, although the symptoms often become present earlier in life.
People with certain rheumatic diseases – such as rheumatoid arthritis, systemic lupus erythematosus (commonly called lupus) or ankylosing spondylitis (spinal arthritis) – may be more likely to have fibromyalgia too.
Several studies indicate that women with a family member with fibromyalgia are more likely to have the condition themselves, but the reason for this – whether it be heredity, shared environmental factors or both – is unknown.What Causes Fibromyalgia?
The causes of fibromyalgia are unknown, but there are probably several factors involved. Many people associate the development of fibromyalgia with a physically or emotionally stressful or traumatic event, such as an automobile accident. Some connect it to repetitive injuries. Others link it to an illness. For others, fibromyalgia seems to occur spontaneously.
Many researchers are examining other causes, including problems with how the central nervous system (the brain and spinal cord) processes pain.
Some scientists speculate that a person’s genes may regulate the way his or her body processes painful stimuli. According to this theory, people with fibromyalgia may have a gene or genes that cause them to react strongly to stimuli that most people would not perceive as painful. There have already been several genes identified that occur more commonly in fibromyalgia patients, and NIAMS-supported researchers are currently looking at other possibilities.
How Is Fibromyalgia Diagnosed?
Research shows that people with fibromyalgia typically see many doctors before receiving the diagnosis. One reason for this may be that pain and fatigue, the main symptoms of fibromyalgia, overlap with those of many other conditions. Therefore, doctors often have to rule out other potential causes of these symptoms before making a fibromyalgia diagnosis.
Also, there are currently no diagnostic laboratory tests for fibromyalgia; standard laboratory tests fail to reveal a physiologic reason for pain. Because there is no generally accepted, objective test for fibromyalgia, some doctors unfortunately may conclude a patient’s pain is not real, or they may say there’s little they can do.
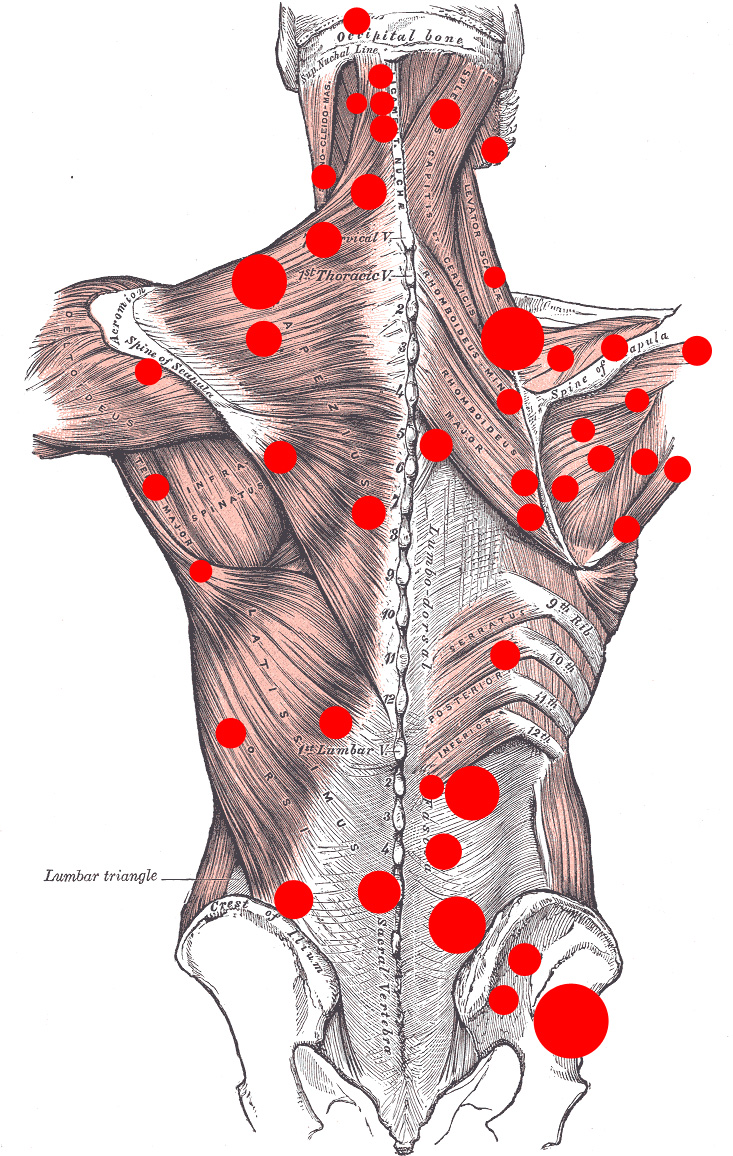
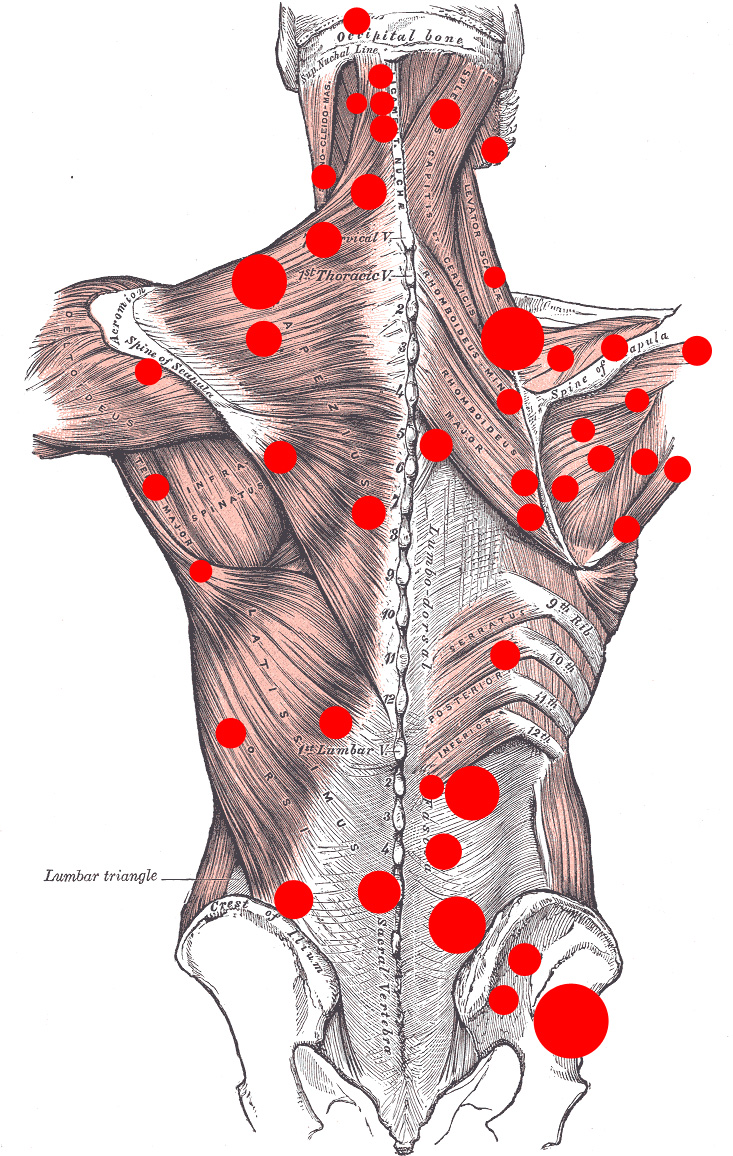
A doctor familiar with fibromyalgia, however, can make a diagnosis based on criteria established by the American College of Rheumatology (ACR): a history of widespread pain lasting more than 3 months, and other general physical symptoms including fatigue, waking unrefreshed, and cognitive (memory or thought) problems.Pain is considered to be widespread when it affects all four quadrants of the body, meaning it must be felt on both the left and right sides as well as above and below the waist. ACR also has designated 18 sites on the body as possible tender points. To meet the strict criteria for a fibromyalgia diagnosis, a person must have 11 or more tender points, but often patients with fibromyalgia will not always be this tender, especially men. People who have fibromyalgia certainly may feel pain at other sites too, but those 18 standard possible sites on the body are the criteria used for classification.
How Is Fibromyalgia Treated?
Fibromyalgia can be difficult to treat. Not all doctors are familiar with fibromyalgia and its treatment, so it is important to find a doctor who is. Many family physicians, general internists or rheumatologists (doctors who specialize in arthritis and other conditions that affect the joints or soft tissues) can treat fibromyalgia.
Fibromyalgia treatment often requires a team approach – with your doctor, a physical therapist, possibly other health professionals and, most importantly, yourself all playing an active role.
It can be hard to assemble this team, and you may struggle to find the right professionals to treat you. When you do, however, the combined expertise of these professionals can help you improve the quality of your life.
You may find several members of the treatment team at pain and rheumatology clinics that specialize in arthritis and other rheumatic diseases, including fibromyalgia.Only three medications – duloxetine, milnacipran and pregabalin – are approved by the U.S. Food and Drug Administration (FDA) for fibromyalgia treatment.
Duloxetine was originally developed for and is still used to treat depression. Milnacipran is similar to a drug used to treat depression but is FDA-approved only for fibromyalgia. Pregabalin is a medication developed to treat neuropathic pain (chronic pain caused by damage to the nervous system).
The following are some of the most commonly used categories of drugs for fibromyalgia:
Analgesics: Analgesics are painkillers. They range from over-the-counter acetaminophen to prescription medicines, such as tramadol and even stronger narcotic preparations. For some people with fibromyalgia, narcotic medications are prescribed for severe muscle pain.
However, there is no solid evidence showing that narcotics actually work to treat the chronic pain of fibromyalgia, and most doctors hesitate to prescribe them for long-term use because of the potential of physical or psychological dependency.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): As their name implies, nonsteroidal anti-inflammatory drugs – including aspirin, ibuprofen and naproxen sodium – treat inflammation. Although inflammation is not a fibromyalgia symptom, NSAIDs also relieve pain. The drugs inhibit substances in the body called prostaglandins, which play a role in pain and inflammation. These medications, some of which are available without a prescription, may help ease the muscle aches of fibromyalgia. They may also relieve menstrual cramps and the headaches often associated with fibromyalgia.Complementary and Alternative Therapies: Many people with fibromyalgia also report varying degrees of success with complementary and alternative therapies, including massage, movement therapies (such as Pilates and the Feldenkrais method), chiropractic treatments, acupuncture, and various herbs and dietary supplements for different fibromyalgia symptoms.
Although some of these supplements are being studied for fibromyalgia, there is little, if any, scientific proof yet that they help. The FDA doesn’t regulate the sale of dietary supplements, so information about side effects, proper dosage and the amount of a preparation’s active ingredient may not be well known.
If you’re using or would like to try a complementary or alternative therapy, you should first speak with your doctor, who may know more about the therapy’s effectiveness, as well as whether it’s safe to try in combination with your medications.
What Can I Do to Try to Feel Better?
Besides taking medicine prescribed by your doctor, there are many things you can do to minimize the impact of fibromyalgia on your life. These include:
Getting better sleep. Getting enough sleep and the right kind of sleep can help ease the pain and fatigue of fibromyalgia. Even so, many people with fibromyalgia have problems such as pain, restless legs syndrome, or brainwave irregularities that interfere with restful sleep. It’s important to discuss any sleep problems with your doctor, who can prescribe or recommend treatment for them.Here are some tips for a better night’s sleep:
- Keep regular sleep habits. Try to get to bed at the same time and get up at the same time every day – even on weekends and vacations.
- Avoid caffeine and alcohol in the late afternoon and evening. If consumed too close to bedtime, the caffeine in coffee, soft drinks, chocolate and some medications can keep you from sleeping or sleeping soundly. Even though it can make you feel sleepy, drinking alcohol around bedtime also can disturb sleep.
- Time your exercise. Regular daytime exercise can improve nighttime sleep. But avoid exercising within 3 hours of bedtime, which actually can be stimulating, keeping you awake.
- Avoid daytime naps. Sleeping in the afternoon can interfere with nighttime sleep. If you feel you can’t get by without a nap, set an alarm for 1 hour. When it goes off, get up and start moving.
- Reserve your bed for sleeping. Watching the late news, reading a suspense novel, or working on your laptop in bed can stimulate you, making it hard to sleep.
- Keep your bedroom dark, quiet and cool.
- Avoid liquids and spicy meals before bed. Heartburn and late-night trips to the bathroom aren’t conducive to good sleep.
- Wind down before bed. Avoid working right up to bedtime. Do relaxing activities, such as listening to soft music or taking a warm bath, that get you ready to sleep. (A warm bath also may soothe aching muscles.)
Exercising. Although pain and fatigue may make exercise and daily activities difficult, it’s crucial to be as physically active as possible. Research has repeatedly shown that regular exercise is one of the most effective treatments for fibromyalgia. People who have too much pain or fatigue to do vigorous exercise should begin with walking or other gentle exercise, and build endurance and intensity slowly.
Making changes at work. Most people with fibromyalgia continue to work, but they may have to make big changes to do so. For example, some people cut down the number of hours they work, switch to a less demanding job, or adapt a current job. If you face obstacles at work, such as an uncomfortable desk chair that leaves your back aching or difficulty lifting heavy boxes or files, your employer may make adaptations that will enable you to keep your job. An occupational therapist can help you design a more comfortable workstation or find more efficient and less painful ways to lift.
Eating well. Although some people with fibromyalgia report feeling better when they eat or avoid certain foods, no specific diet has been proven to influence fibromyalgia. Of course, it’s important to have a healthy, balanced diet. Not only will proper nutrition give you more energy and make you generally feel better, it will also help you avoid other health problems.
From the National Institutes of Health
Published May 15, 2014
by admin | Apr 24, 2015 | Uncategorized
Fibromyalgia Syndrome: Mystery Pain Explained
Painful and puzzling, fibromyalgia syndrome primarily strikes women. Why? Researchers don’t know. And with details scarce about its cause and treatment, dealing with the condition can be maddening. We have answers to 10 common questions about fibromyalgia in women…
1. What causes fibromyalgia syndrome?
Genetics may play a role in developing fibromyalgia. But no one really knows what causes the syndrome and there are no known risk factors.
The most prevalent theory is that fibromyalgia results from a disturbance in the central nervous system called central sensitization, which may intensify pain signals.
Linked to that theory is the notion that patients have higher amounts of a compound called substance P in their spinal fluid, which increases their sensitivity to pain.
Another theory: There may be two types of fibromyalgia: “primary” fibromyalgia, which occurs spontaneously, and “secondary” fibromyalgia, which may be triggered by trauma – such as a car accident – or by certain infections, such as Lyme disease and hepatitis C.Some researchers think that the primary type is caused by a sleep disturbance, but it’s also possible that the sleep disturbance is a symptom of fibromyalgia.
2. I often hear fibromyalgia, chronic fatigue syndrome and lupus mentioned together. Are they similar?
Although the three are separate conditions, symptoms of fibromyalgia and chronic fatigue syndrome overlap. And fibromyalgia and lupus both involve the muscle and bone network in our bodies, which can cause confusion between the two illnesses.
Fibromyalgia is characterized by many symptoms including muscle pain, fatigue, sleep disturbances, irritable bowel syndrome and, in some people, depression.
Despite its consistent general characteristics, it can be tough to diagnose because symptoms vary from patient to patient.The main symptoms of chronic fatigue syndrome (CFS) include:
- Overwhelming fatigue
- Memory loss
- Muscle soreness
- Sore throat
- Swollen glands
Symptoms can coincide or come and go in individual cycles. Doctors usually diagnose CFS through a process of elimination: They rule out other potential causes of long-term fatigue.
Lupus is an autoimmune disease in which the body attacks itself. It may start with joint pains, which patients can confuse with the muscle pains of fibromyalgia.
Diagnosed by blood tests that show a high level of certain antibodies, lupus can be progressive and cause serious illness throughout the body.
People with lupus appear more prone to develop fibromyalgia and chronic fatigue, although researchers don’t know why.
3. Why do more women than men get fibromyalgia syndrome?
The majority of people with fibromyalgia (80%-90%) are women, as is the case with lupus and CFS.
No one knows why women are affected more often than men.
4. Is it age-related?
Fibromyalgia occurs most commonly in people between 20 and 55 years old, although it may arrive at any age, including childhood.
5. Is it an autoimmune disease or a form of arthritis?
Neither. In fact, unlike inflammatory arthritis and autoimmune disease, which cause joint destruction and inflammation, fibromyalgia causes neither, despite symptoms of joint and muscle pain.
6. What are warning signs or symptoms of fibromyalgia?
Alas, the symptoms of fibromyalgia arrive without warning. They can, as mentioned earlier, include muscle and joint soreness, fatigue, sleep problems, irritable bowel symptoms, morning stiffness, depression and brain fog.
7. How is it diagnosed?
Unfortunately, it’s not uncommon to be misdiagnosed or have to see several doctors before a diagnosis is made.
Your best bet is to see a rheumatologist, a doctor who specializes in conditions affecting muscles and joints.
He or she will look for symptoms and physical findings that meet a specific definition of fibromyalgia established by the American College of Rheumatology.For example, a patient must have 11 out of 18 specific tender points on her body (neck, shoulders, back, hips, and upper and lower extremities), and she must have had widespread pain in her muscles and joints lasting for three months or more without explanation.
The doctor will also work to rule out other diseases that have similar symptoms, such as lupus and polymyalgia rheumatica (another autoimmune disease).
8. What lifestyle changes can I make to help alleviate the symptoms?
Get plenty of gentle aerobic exercise (like swimming or walking briskly), working up to at least 30 minutes most days of the week.
Weight gain commonly accompanies fibromyalgia (thanks to the fatigue, muscle pain and poor sleep).
Regular exercise will give you more energy, boost your mood, lower your weight and help you sleep better.
Eating a healthy diet with lots of vegetables, fruits, whole grains, lean meats and dairyalso will energize you, lower your weight and improve your overall health as you battle fibromyalgia.You can also try eliminating the following foods, which appear to bother some people with fibromyalgia:
- Food additives like MSG and nitrates (the preservative in hot dogs and bacon)
- Aspartame (NutraSweet)
- Sugar
- Caffeine drinks
But remember, what works for one person may not work for another.
9. What are the latest fibromyalgia treatments?
Pregabalin (Lyrica) was the first to be approved by the Food and Drug Administration (FDA) for fibromyalgia [in 2007]. Studies suggest that it prevents pain and improves sleep by slowing the release of chemicals associated with pain. [Duloxetine (Cymbalta) was approved in 2008 and Milnacipran (Savella) in 2009.]
Older standbys can help too. Anti-inflammatories such as ibuprofen and muscle relaxers can relieve pain. Antidepressants – especially tricyclics (amitriptyline or Elavil) – boost mood as well as lessen pain and improve sleep.Supplements such as 5-HTP and SAM-e (S-adenosylmethionine) may also be useful. An amino acid, 5-HTP, converts to serotonin, a feel-good neurotransmitter that helps boost mood and sleep. SAM-e is an enzyme already present in the body that affects mood and lessens pain.
D-Ribose, a simple sugar in powder form, may lessen pain and fatigue when dissolved in water and taken 2-3 times daily.
Cognitive behavioral therapy, acupuncture, hypnotherapy and biofeedback may also be worth trying.
10. What is the long-term outlook for a woman with fibromyalgia?
The good news is that fibromyalgia does not cause damage to muscles and joints that can lead to debilitation, immobility or joint replacement.
The bad news is that the symptoms typically don’t resolve. Many women simply must learn to live with fibromyalgia.
The key is finding individual or combination therapies that help. Not all treatments help all patients with fibromyalgia; discovering which help you is a matter of trial and error. But scientists continue to work on finding the cause of fibromyalgia and, ultimately, a cure or effective treatment.
How Much Do You Know About Fibromyalgia?
Described by Hippocrates in ancient Greece, fibromyalgia is one of the world’s oldest medical mysteries. The disease – a complex illness marked by chronic muscle, tendon and ligament pain, fatigue and multiple tender points on the body – affects about 2% percent of Americans, most of them women.
By Robin H. Miller, M.D. and Janet Horn, M.D., Lifescript Women’s Health Experts
Published April 16, 2015