by admin | Jan 9, 2015 | Uncategorized
Introduction
Radiofrequency ablation is a term used when radio waves are used to produce heat to destroy tissue, usually a nerve. It has been used for several years with great success in patients who have abnormally fast heartbeats. More recently, it is being used to destroy tumors. It is a non-surgical option to treat your spine pain.
Spine pain is the second most frequent pain complaint. It occurs in 65 to 80 percent of the population at one time or another, and can be disabling and frightening. Its costs to society are great.
In the case of spinal pain, radiofrequency waves are transmitted through a needle placed into the facet joint under x-ray guidance. This procedure is also known as rhizotomy.
This guide will help you understand
- What parts of the spine are involved
- What is the surgeon is trying to achieve
- What happens during the procedure
- What are the possible complications
Anatomy
What parts make up the spine?
The spine is made up of three general parts. The top portion is the cervical spine and connects with the skull or cranium. The middle portion is the thoracic spine and is identified by the ribs that attach to each of the vertebrae. The lower portion is the lumbar spine. It connects with the pelvis at the sacrum.
The human spine is made up of 24 spinal bones called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
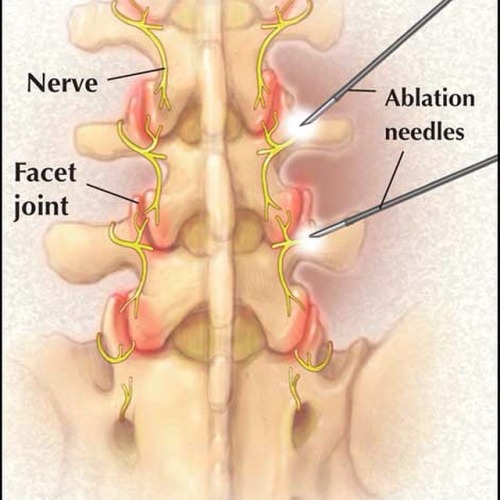
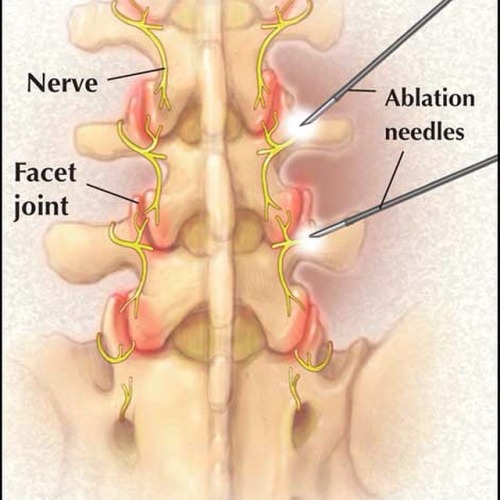
The vertebrae have discs that serve as cushions in between them. Each vertebra has two sets of bony knobs that meet between each vertebra. These form facet joints. The facet joints are located on the back of the spinal column in the lumbar and thoracic spine. In the neck, or cervical spine, they are located on each side of the vertebra. They are also called zygoaphophyseal or apophyseal joints.
A joint is where two or more bones are joined, allowing motion. Facet joints allow flexion or forward bending, and extension or backward bending, as well as rotation of your spine. The facet joints are synovial joints. This means that a capsule of soft tissue encloses them to help support it. It also makes fluid that lubricates the joint, like oil for the moving parts of a machine.
The surfaces of the joints are lined with cartilage. This allows joints to move or glide smoothly. The articular cartilage surface of the facet joint can become thin due to wear and tear. Bone spurs and enlargement of the joint can occur due to chronic inflammation and arthritis.
Nerves called medial branches supply facet joints. They carry the pain signals to the spinal cord. The signals eventually reach the brain where the pain is registered. Pain is a warning when the joint is irritated.
Rationale
What do surgeons hope to achieve with this procedure?
There are several structures in the spine that can be a source of pain. One of the most common sources is the facet joint. The joints can develop arthritis and cause acute and chronic pain. The pain may come and go depending on activity.
Facet joint pain as the cause of back pain can be determined by a facet joint injection. This is called a diagnostic injection, meaning the doctor uses it to help make a diagnosis. The physician using x-ray guidance will inject the facet joint(s) in question with a small amount of a combination of local anesthetic and cortisone. Relief of the acute or chronic problem while the joint is numb indicates that you will likely have a good response to radiofrequency ablation.
Radiofrequency ablation uses radio waves to produce heat to destroy the nerve(s) carrying the pain signals from the facet joint. Once the nerves carrying pain sensation from the joints are destroyed, your pain should be reduced. This should allow you to do more activity, and decrease your pain medications.
Preparation
How should I prepare for the surgery?
Your surgeon will discuss the preoperative guidelines. Follow your surgeon’s instructions. These instructions may include
- Do not eat or drink for at least six hours before the procedure. You will be able to take your usual medication with a small amount of water. If you have diabetes, do not take your insulin or diabetic pills until after the procedure
- You will need a driver to return home
- Do not take any aspirin or aspirin-containing medication at least eleven days before the procedure. They may prolong bleeding
- Wear loose fitting clothing that is easy to take off and put on
- Take a shower the morning of the procedure, using a bactericidal soap to reduce chances of infection
- Do not wear jewelry
Procedure
What happens during the procedure?
When the procedure is to begin, an IV will be started. This will allow the use of medications to help sedate you and make the procedure more comfortable. It is also important to have IV access for medications if you should have an allergic reaction during the procedure.
You should be awake for the procedure to help the doctor with correct placement of the electrode used for radiofrequency ablation. You will not be given a general anesthetic. The area to be treated will be cleaned and then numbed with a local anesthetic.
Using x-ray guidance, the doctor will place the needle in the proper facet joint. A microelectrode is then placed inside the needle. A small radiofrequency current is then sent to the medial branch nerve of the joint capsule for approximately 60 to 90 seconds. The procedure is done with sterile technique to minimize the risk of infection.
After the procedure, you will be taken to a recovery area. The nurses will monitor you and be sure you do not have an allergic reaction. You will be allowed to leave once you are stable.
Complications
What might go wrong?
This procedure is a safe, non-surgical treatment, and the risks for complications are low. However there are several complications that may occur during or after this procedure. No procedure is 100 percent foolproof. This article doesn’t provide a complete list of all the possible complication, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur. Some of the most common complications following radiofrequency ablation include
- Neuritis
- Neuroma
- Numbness-nerve damage
- Infection
- Allergic reaction
- Lack of pain relief
Neuritis
Neuritis is an inflammation of the nerve with pain and tenderness that lasts three to six weeks. This can occur in 10 to 15 percent of patients. Neuritis usually goes away by itself. If it doesn’t, the doctor can inject a local anesthetic along with a steroid into the nerve. Pulsed radiofrequency can also be used to help with the pain and inflammation.
Neuroma
A neuroma is a tumor from a nerve made of nerve cells and fibers. It forms around the area destroyed during radiofrequency ablation. The tumor can put pressure on the nerve and nearby tissue causing increased pain.
Numbness
Numbness caused by nerve damage can occur. Permanent numbness is also a possible complication.
Infection
Infections can also happen. Infections can involve the skin, or the joint and surrounding bone.
Allergic Reaction
Allergic reactions can occur since medications and sometimes contrast dye is used during the procedure. Anaphylaxis is an allergic reaction that is serious and can result in death.
Lack of Pain Relief
Even though a test block was beneficial, some patients have no pain relief from the procedure.
After Care
What should I expect after surgery?
Immediately following the procedure, you may have some relief of pain from the numbing medication used during the procedure.
You will not be able to drive or do any physical activity for 24 hours.
You may experience an increase in pain for the first several days following the procedure. Additional pain medications may be necessary to make you comfortable. If these include narcotics, you will need to watch for constipation. Drink lots of fluids and eat foods with plenty of fiber. If constipation should occur you will need to use a laxative, available over-the-counter.
You may also note some swelling and bruising where the needle was inserted. Using a cold pack may ease the discomfort. Occasionally infection or bleeding can occur at the site of the procedure. If you have a fever of 101 degrees or greater, chills, or redness or drainage at the treatment site, call your doctor.
The degree of pain relief varies from person to person. The maximum decrease in pain may take up to three or more weeks to occur. You can eventually expect 50 percent or greater pain relief. Pain relief can last from six to12 months or even longer. The nerves do repair themselves and your pain may return. The procedure may be done again.
Your doctor will arrange a follow-up appointment, or phone consult within three to four weeks after the procedure to see how you are doing.
Rehabilitation
What should I expect during my rehabilitation?
It is important that you start a program of conditioning, strengthening, and range of motion exercises after radiofrequency ablation. Ideally, increased muscle strength around the arthritic joints will make them less painful for several months after radiofrequency ablation.

by admin | Jan 8, 2015 | Uncategorized
Migraine Relief: 10 Myths and Facts
By Diane Wedner
Migraines are more than just bad headaches. But many people – and even some doctors – don’t fully understand this complex condition or what’s required for migraine pain relief.
You wake up to throbbing pain on one side of your head. The sun streaming through the bedroom window scorches your eyes like a lightning flash. Moving your head even slightly is excruciating.
Like 35 million other Americans, you’re in the throes of a migraine – the most common cause of disabling headaches. About 18% of women and 6% of men experience the brain disorder, according to the Migraine Research Foundation (MRF), a Manhattan-based nonprofit organization that provides information and support.
Even some physicians don’t recognize the cluster of symptoms that makes up migraines – such as headache, nausea, vomiting, visual disturbances and sensitivity to noises and smells. As a result, they may dismiss a severe migraine headache and other symptoms as “women’s problems,” such as premenstrual syndrome (PMS) or depression.
“Because the problem is related to their head, patients sometimes feel that doctors think they’re making the symptoms up, causing their own headaches, or overreacting,” says Cathy Glaser, MRF co-founder and president.
Lack of training is a pervasive problem, says neurologist Peter Goadsby, M.D., Ph.D., director of the University of California, San Francisco Headache Program.
“If physicians aren’t exposed to current information, they have to fill in the blanks themselves,” he explains.
The result: Along with debilitating symptoms, migraine patients often endure a variety of myths about the condition.
If you suffer from migraines, it’s important to stay informed.
Migraine pain myth #1: Migraines are just bad headaches.
Reality check: Not so! Migraine is a syndrome in which “multiple symptoms often occur simultaneously because of a cascade of brain events,” says Joel R. Saper, M.D., director of the Michigan Head-Pain & Neurological Institute in Ann Arbor, Mich.
Those brain events release pain-producing inflammatory substances around the nerves and blood vessels of the head.
The cause is unknown, but the result isn’t: Disabling symptoms that often send sufferers to bed.
Interestingly, some people don’t have pain, though severe pain is the most common symptom of a migraine. In such cases, people often have visual auras and other migraine symptoms, such as nausea.
“But if they do [have pain], it might be minor compared to the drama of nausea, stroke-like symptoms and memory changes,” Dr. Saper says.
Though ordinary headaches result from a narrowing of blood vessels and can often be eased with aspirin, migraines are caused by the expansion of blood vessels. Certain treatments may provide migraine relief, but there’s no cure.
Migraine pain myth #2: Migraines occur only in women.
Reality check: Under age 12, an equal number of boys and girls have migraines, Dr. Saper says. After the onset of puberty, men still get them, but women with the condition outnumber them 3-1. The main reason is estrogen and progesterone, which play a significant role in the disorder, according to epidemiological and clinical studies.
The two hormones help regulate pregnancy, during which migraines may “settle down,” Dr. Goadsby says. Menopause may also bring migraine relief, he adds.
Higher estrogen levels sometimes improve migraines, while lower levels may make them worse, according to the Mayo Clinic in Rochester, Minn.
Some women get their first migraine headache after starting on birth control pills; for others, oral contraceptives improve the headache pattern, the clinic says.
Migraine pain myth #3: Premenstrual syndrome (PMS) causes migraines. Reality cheek: The two conditions are sometimes connected, but “not all women with periods have PMS, and not all women with migraines have PMS,” Dr. Saper says. Migraines are sensitive to hormonal fluctuations, which occur before a woman’s period. An attack that comes within two days before or three days after a period, known as a “menstrual migraine,” is similar to other migraines but usually doesn’t include an aura (visual disturbances).
Women who experience menstrual migraines can sometimes get relief from continuous birth control pills, which reduce the number of periods to four per year.
Here are other treatments for menstrua] migraines.
Migraine pain myth #4: Women get migraines because they’re more emotional. Reality check: “That’s nonsense,” Dr. Goadsby says. “The ‘hysterical female’ argument is embarrassing.”
“Women, like men, get migraines because something’s going on in their brains,” says Glaser of the MRF. “They’re usually born with that trait. The question is: If you have the trait, what triggers the migraine?”
For both men and women, emotional stress may release chemicals that provoke migraine-causing vascular expansion in the brain, according to Harvard Medical School’s Beth Israel Deaconess Medical Center (BIDMC).
“If life is stressful – you have a bad marriage, you’re hurt – you may be more vulnerable to migraines,” Dr. Saper says.
The letdown after a stressful period also may be a migraine trigger.
Remember, though, that “lots of women are stressed and don’t get migraines,” Glaser says. “You have to have the trait.”
Migraine pain myth #5: Painkillers are enough for migraine relief.
Reality check: Because migraines can provoke multiple symptoms, one pain medicine won’t necessarily sweep them away, Dr. Goadsby says.
“There are more than 100 treatments and prevention methods for migraines,” Glaser says. “If patients could pop just one pill, they’d be doing it.”
Although painkillers often are prescribed for migraines, they’re not the most effective treatment, experts say. They don’t work, for example, against triggers such as movement or noise, which may exacerbate symptoms.
Other medications can target symptoms in addition to migraine headache. But some have serious side effects, especially if patients also use painkillers regularly.
“The more painkillers you take, the greater the potential for more headaches,” Dr. Saper says.
Called medication overuse headaches, or rebound headaches, these are more like tension headaches than migraines, Dr. Saper says. Using painkillers 2-3 times weekly over several months may make patients more vulnerable to them. There are serious health dangers from painkiller overuse.
Pain relievers such as ibuprofen (Advil) and acetaminophen (Tylenol) help relieve mild migraine symptoms, but they shouldn’t be used to treat moderate or severe migraines, according to the Mayo Clinic.
Synthetic narcotics known as opioids, such as hydrocodone (Vicodin), can be more effective, but they “change the nervous system and make it easier to get the next attack,” Dr. Saper warns. They also can be addictive.
Other drags may help patients with more severe symptoms, including:
- Triptans: They work with brain chemistry to constrict blood vessels, helping relieve migraine pain, nausea and sensitivity to light and sound.
- Ergot: These combine caffeine with ergotamine, another blood-vessel constrictor, and work best in patients who have pain lasting more than 48 hours.
- Dexamethasone: This corticosteroid reduces inflammation and maybe used with other medications for migraine pain relief; it’s taken infrequently because of the risk of side effects.
- Tricyclic antidepressants: This form of antidepressant medication may help prevent migraines by altering brain chemistry, whether or not you have depression.
- Beta blockers: Commonly used to treat high blood pressure and coronary heart disease, these drags reduce the frequency and severity of migraines.
- Anti-nausea medications: These help with the migraine symptoms of nausea and vomiting.
There’s another drag treatment that you may not be aware of — one popularly known to fight wrinkles:
Following two clinical studies published in the medical journal Cephalalgia in 2010, the FDA approved Botox (OnabotulinumtoximA) for the treatment of chronic migraine headaches.
The studies were double-blind, randomized, placebo-controlled with more than 1,300 study participants. At the end of the two clinical trials, the researchers concluded that Botox is safe and effective, for the prevention of chronic migraines in adults.
Multiple studies since have shown the continuing effectiveness of Botox treatment for chronic migraines.
New treatments for migraine sufferers are emerging all the time. The latest was just announced by the FDA in March 2014. It is the first medical device approved to prevent migraines in adults, providing an alternative to medication.
According to the FDA, Cefaly is a small, portable, battery-powered, prescription device that resembles a plastic headband worn across the forehead and atop the ears. The user positions the device in the center of the forehead, just above the eyes, using a self-adhesive electrode.
The device applies an electric current to the skin and underlying body tissues to stimulate branches of the trigeminal nerve, which has been associated with migraine headaches. The user may feel a tingling or massaging sensation where the electrode is applied. It is directed for use once per day for 20 minutes.
Migraine pain myth #6: Migraines aren’t hereditary.
Reality check: The child of one parent with migraines has a 50% chance of having them too, and the risk climbs to 75% if both parents experience them, according to BIDMC. The risk is 20% if even a distant relative has the disorder.
A boy may inherit the gene, but is less likely to get migraines, Dr. Goadsby says. But he can pass the trait on to his daughters, who are more likely to experience symptoms.
Migraine pain myth #7: Migraines are caused by psychological problems.
Reality check: Migraines, depression and anxiety often travel together. The causes may overlap – a
risk of depression, for example, can also be hereditary – but one condition doesn’t lead to the others.
Not everyone with depression gets migraines, and vice versa, Dr. Saper says.
“You can treat someone with depression with antidepressants, but that doesn’t mean it will help the migraine,” Dr. Goadsby says. And “you can give anti-migraine medications to a migraine patient, but she’ll still have depressive disorder.”
“The two are related only by shared brain chemistry,” he says.
Migraine pain myth #8: Caffeine helps relieve migraines.
Reality check: It helps some people – but for others, it’s a migraine trigger, according to BIDMC.
Caffeine can help relieve a mild or moderate migraine headache if you don’t consume much of it daily, Dr. Saper says.
But 4-5 cups of coffee per day may foster a caffeine dependency, and overnight withdrawal from the stimulant could trigger a migraine the next morning.
To help determine whether caffeine affects your condition, keep a headache diary to note if you get migraine symptoms after consuming caffeinated beverages, BIDMC suggests.
Migraine pain myth #9: Certain foods trigger migraines. Reality check: Some migraine patients are sensitive to:
Cheese, which contains a natural compound called tyramine
Chocolate, which has caffeine
Processed meats made with nitrates
But many others never suffer a migraine headache from food, Dr. Saper says. “It could be 100 different triggers,” he says. “It’s hard to identify them.”
If you often get symptoms after eating a particular food, keep a diary to track what you’ve eaten when you develop symptoms, Glaser advises. These 5 foods can ease migraines.
It also matters when you eat. Inconsistent mealtimes can set off migraines.
“Eat at the same time every day,” Dr. Saper advises. “Missing or delaying meals are often a key migraine trigger.”
Exercising and going to bed at the same time daily is also wise, he adds.
Migraine pain myth #10: Overachieving women get migraines from too much multitasking.
Reality check: Stress can be a migraine trigger, but “it doesn’t matter whether a woman is under stress in an office or at home with kids,” Dr. Goadsby says.
Stress-reducing techniques, such as meditation, may help manage migraines.
It isn’t just a women’s issue either.
“It’s a myth that stress applies to women more than men,” Dr. Saper says.
Don’t let this, or any other migraine myth, deter you from living your life and getting proper treatment, Dr. Goadsby says.
“You’re not crazy, weak or second-rate if you have migraines,” he says. “You have a genuine, biologically determined problem. Don’t believe anything else.”

by admin | Jan 8, 2015 | Uncategorized
Intravenous Infusion Therapy
Intravenous (IV) infusion therapy is an exciting treatment option for numerous pain syndromes ranging from fibromyalgia and small fiber neuropathy to Complex Regional Pain Syndrome (CRPS) and Reflex Sympathetic Dystrophy (RSD). IV infusion therapy is very simple: an IV line is placed in the patient’s arm and the medication flows in.
There are several medications that are commonly delivered IV for pain management:
• Lidocaine
• Ketamine
• Immunoglobulin (IG)
• Clonidine
• Dexmedetomidine
• Bisphosphonates
• Magnesium
These medications are typically mixed with saline in an IV bag and slowly infused accordingly based on the medication and/or protocol being utilized.
Procedure Overview

Dr. Hanna will first select the appropriate medication to be used in the infusion depending on the type of pain that you are experiencing. Next, the office staff will weigh you to determine the proper amount of medication needed and mix it with saline in an IV bag. Next, Dr. Hanna will place an IV line in your arm or hand per standard IV protocols. The medication is infused through the IV over variable times depending on the medication. It’s that simple. During the infusion process, you will be placed on a monitor and your vitals will be closely observed for the duration of the infusion.
Medication Overview
Lidocaine – Blocks sodium channels in the neuronal cell membrane that may potentially play a role in the pathogenesis and maintenance of both neuropathic and inflammatory pain
Ketamine – N-methyl-D-aspartate (NMDA) Receptor antagonist – therefore decreases sustained neuronal depolarization and excitatory transmission along afferent pain pathways in the dorsal horn of the spinal cord
Immunoglobulin (IG) – Counteracts neuroinflammation by inhibiting complement deposition, neutralizing cytokines and growth factors, speeds up clearance of potentially pain-inducing auto-antibodies, and activation of macrophages and T cells through FcγRIIb receptor
Clonidine – α2-adrenergic receptor agonist believed to reduce of norepinephrine release from the α2-adrenergic in the periphery
Dexmedetomidine – Selective α2-adrenergic agonist that may have a role in treating painful conditions that are manipulated and/or attenuated by the sympathetic nervous system
Bisphosphonates – Decreases neuropathic bone pain by suppressing bone resorption via osteoclast inhibition, shortens osteoclast life span and decreasing the acidity of the local microenvironment
Magnesium – Competitive NMDA receptor antagonist that decreases acute and chronic pain by stabilizing abnormal nerve excitation
How Many Treatments are Required?
The response to treatment varies patient by patient. Most require several treatments; the amount required depends on the medication and the protocol being used. Some people respond at first infusion, but most will not feel the full benefit until several treatments have been administered.
Is Infusion Therapy Right for me?
If you suffer from chronic pain that has not responded to medication or other traditional treatment options, then infusion therapy may be an option for you.
To make an appointment today with Dr. Hanna, call 727-797-7463.