by admin | May 5, 2015 | Uncategorized
Weekly Breaking Research Updates
Scientific breakthroughs happen every day! In an effort to help our patients stay up to speed on the most cutting edge treatment options available for them, our scientists monitor current research and publish weekly research updates. The title of each article below is a link to the full study report. If you’d like to make an appointment with Dr. Hanna to discuss your treatment options, please contact us.
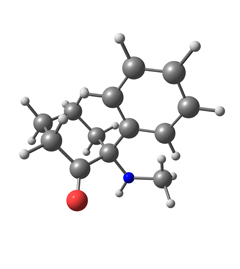
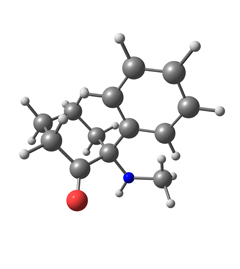
Ketamine
Ketamine-A Narrative Review of Its Uses in Medicine.
BM Radvansky, S Puri, AN Sifonios, JD Eloy, V Le – American Journal of Therapeutics, 2015
One of the most fascinating drugs in the anesthesiologist’s armament is ketamine, an N-
methyl-D-aspartate receptor antagonist with a myriad of uses. The drug is a dissociative
anesthetic and has been used more often as an analgesic in numerous hospital units, …
Acute administration of ketamine inhibited stress induced pro-inflammatory cytokines in hippocampus of rats
G Unal, G Terzioglu, C Sahin, GY Demirel, F Aricioglu – Bulletin of Clinical …, 2015
Objective: Major depression is a complex and devastating disease which one-third of
patients still do not respond to current treatments. It has been demonstrated that there is a
correlation between high levels of plasma cytokines such as IL-1β, IL-6, IL-18 and TNF-α …
The Efficacy and Safety of Procedural Sedoanalgesia with Midazolam and Ketamine in Pediatric Hematology.
GS Aylan, N Sarper, U Demirsoy, E Zengin, E Çakmak – Turkish journal of …, 2015
OBJECTIVE: The aim of this study is to investigate the efficacy and safety of sedoanalgesia
performed outside the operating room by pediatricians trained in advanced airway
management and life support. MATERIALS AND METHODS: Midazolam and ketamine …
[HTML] Alpha-lipoic acid alone and combined with clozapine reverses schizophrenia-like symptoms induced by ketamine in mice: Participation of antioxidant, nitrergic and …
GS Vasconcelos, NC Ximenes, CNS de Sousa… – Schizophrenia Research, 2015
Abstract Oxidative stress has important implications in schizophrenia. Alpha-lipoic acid
(ALA) is a natural antioxidant synthesized in human tissues with clinical uses. We studied
the effect of ALA or clozapine (CLZ) alone or in combination in the reversal of …
Low Dose Ketamine Infusion For Managing Acute Pain
M Yetim, S Tekindur, Y Emrah Eyi – The American Journal of Emergency Medicine, 2015
Dear Editor, We read with great interest the article “Short (low-dose) ketamine infusion for
managing acute pain in the ED: case-report series” written by Goltser et al (1). We believe
that this original study provides a new and insightful approach to pain management in …
[PDF] Symptomatic remission and hippocampus volume in schizophrenia
PT Chang, JF Lirng, YH Chou – Bulletin of Clinical Psychopharmacology, 2015
… 1):S146-S7 [Abstract:0577] Neuroimaging in psychiatry Alterations in resting state electrocortical
network oscillations, schizophrenia-like symptoms and their relationships induced with the
administration of the NMDA receptor antagonist ketamine in human volunteers …
G535 (P) The development and implementation of a policy promoting parental (patient) involvement in escalation of clinical care
MA Webster, C Haines, J Fraser – Archives of Disease in Childhood, 2015
… www.midstaffspublicinquiry.com/report (accessed 28 Nov 2014) G536(P) THE CHALLENGES
OF SETTING UP A KETAMINE SEDATION SERVICE IN THE PAEDIATRIC ED – LEARNING
LESSONS AND EFFECTING CHANGE 1E Dewhirst, 1C Whitehouse, 2T Waterfield. …
[PDF] Eyes tell the psychopathology: preliminary findings
H Balibey, C Basoglu, A Ates, A Algul, R Tutuncu… – Bulletin of Clinical …, 2015
… On the other hand, the behavioral and pharmacological effects of the noncompetitive
N-methyl-D-aspartate (NMDA) receptor antagonist ketamine have been used to study
important aspects of psychotomimetic action in humans. …
Adjunctive Use of Ceftriaxone and Sodium Valproate in the Management of Tetanus: A Case Report and Literature Review
S Oriaifo, N Oriaifo, M Oriaifo, E Okogbenin, E Omogbai – Journal of Biology, …, 2015
… immune globulin. Control of spasms was mainly by the use of the GABAergic-
enhancing drugs diazepam and sodium valproate combined with the use of the
anti-excitotoxics magnesium sulphate and ketamine. The introduction …
PyBidine–NiCl2-Catalyzed Asymmetric Addition of Alcohols and Peroxides to Isatin-Derived Ketimines
T Arai, K Tsuchiya, E Matsumura – Organic Letters, 2015
… adduct (27%, 80% ee). The formation of the chiral N,O-acetal inspired us to optimize
the reaction conditions for the addition of methanol to an isatin-derived
N-Boc-ketamine (1a), as shown in Table 1. Table 1. Optimization of …
Radiofrequency Ablation (RFA)
Radiofrequency Ablation for Atrial Fibrillation: Trends in Patients, Clinical Outcomes, and Resources Among Medicare Beneficiaries from Fiscal Year 2010 to Fiscal …
MR Reynolds, AD Kugelmass, DJ Cohen, PP Brown… – … : Cardiovascular Quality and …, 2015
Abstract Introduction: The objective of this analysis was to report four year trends among
Medicare beneficiaries (MB) undergoing Radiofrequency Ablation (RFA) to treat Atrial
Fibrillation (AF). Methods: This retrospective study examined both the Medicare Provider …
Systematic review and meta-analysis of perinatal outcomes following radiofrequency ablation and bipolar cord occlusion in monochorionic pregnancies
K Gaerty, RM Greer, S Kumar – American Journal of Obstetrics and Gynecology, 2015
Objective The aim of this study was to analyse perinatal outcomes following selective
reduction in monochorionic pregnancies using either radiofrequency ablation (RFA) or
bipolar cord occlusion (BCO). Study Design This was a systematic review and meta- …
Sublobar Resection, Radiofrequency Ablation or Radiotherapy in Stage I Non-Small Cell Lung Cancer
S Safi, G Rauch, J Kunz, T Schneider, M Bischof… – Respiration, 2015
Background: The best therapy for patients with stage I non-small cell lung cancer (NSCLC)
who are medically unfit for lobectomy or prefer not to undergo surgery has not yet been
demonstrated. Objectives: We analyzed data from our prospective database to evaluate …
The efficacy of radio-frequency ablation for metastatic lung or liver tumors of male germ cell tumors as an alternative minimally invasive therapy after salvage …
Y Naya, T Nakamura, M Oishi, T Ueda, H Nakanishi… – International Journal of …, 2015
… Okuma et al. [14] reported that tumors under 20 mm in size can be completely ablated in lung
tumor. … Cancer 3:1409–1419 7. Curley SA, Izzo F, Delrio P et al (1999) Radiofrequency ablation
of unresectable primary and metastatic hepatic malignancies. Results in 123 patients. …
Metastastectomy for metachronous pulmonary and hepatic metastases from nasopharyngeal carcinoma: Report of 6 cases and review of the literature
SJM Lim, NG Iyer, LL Ooi, HN Koong, A Chung, HK Tan… – Head & Neck, 2015
… not prevent disease progression in the long term. Surgery and radiofrequency ablation have … ten
patients who underwent radiofrequency ablation +/- adjuvant chemotherapy had a median survival
period of 77.1 months compared to 32.4 months in another ten patients who only …
[HTML] Lobulated Enhancement Evaluation in the Follow-Up of Liver Metastases Treated by Stereotactic Body Radiation Therapy
H Jarraya, P Borde, X Mirabel, O Ernst, T Boulanger… – International Journal of …, 2015
… have limitations for the evaluation of targeted therapies; for example, imatinib for gastrointestinal
stromal tumors (GIST) and bevacizumab for colorectal liver metastasis 8, 9 and 10 or other local
treatments, such as lung tumor SBRT (11), liver radiofrequency ablation (12), and …
Percutaneous microwave ablation of thyroid nodules: effects on thyroid function and antibodies
K Heck, C Happel, F Grünwald, H Korkusuz – International Journal of Hyperthermia, 2015
… The results demonstrated that in all 30 sessions the complete volume of the 34
nodules could be ablated. The treatment … al. Radiofrequency ablation of benign thyroid
nodules: Safety and imaging follow-up in 236 patients. Eur …
Current state of the treatment of perforating veins
ED Dillavou, M Harlander-Locke, N Labropoulos… – Journal of Vascular Surgery: …, 2015
… Table II. Technical success of radiofrequency ablation (RFA), endovenous laser ablation (EVLA),
and ultrasound-guided foam sclerotherapy (UGFS). Primary author (year), Perforator treatment
modality, No. … 14, 15, 18 and 26. Radiofrequency ablation (RFA). …
Irreversible Electroporation of the Pancreas Is Feasible and Safe in a Porcine Survival Model.
S Fritz, CM Sommer, D Vollherbst, MF Wachter… – Pancreas, 2015
… From a histopathological point of view, the ablated area was character- ized by cellular eosinophila …
The ability of IRE to ablate undesirable tissue near large blood vessels and damageable … of the
electric field to which the tissue is exposed.13 Radiofrequency ablation has been …
An Analysis of Patients Transferred to a Tertiary Oncological Intensive Care Unit for Defined Procedures
S Kamat, S Chawla, P Rajendram, SM Pastores… – American Journal of Critical …, 2015
Skip to main page content. …
Complex Regional Pain Syndrome (CRPS/RSD)
Two Virtual Reality Pilot Studies for the Treatment of Pediatric CRPS
AS Won, CA Tataru, CM Cojocaru, EJ Krane… – Pain Medicine, 2015
… Letter to the Editor. Two Virtual Reality Pilot Studies for the Treatment of Pediatric CRPS. … How
to Cite. Won, AS, Tataru, CA, Cojocaru, CM, Krane, EJ, Bailenson, JN, Niswonger, S. and Golianu,
B. (2015), Two Virtual Reality Pilot Studies for the Treatment of Pediatric CRPS. …
A dynamic PUF anti-aging authentication system based on restrict race code
B Li, S Chen – Science China Information Sciences, 2015
… Based on the CRP mechanism, the PUF circuit can produce chip-unique responses when
challenges are applied to it and stored in the database by the way of CRPs. (2) Authentication. …
The expected data in the database are called CRPs in paper. …
Increased prevalence of two mitochondrial DNA polymorphisms in functional disease: Are we describing different parts of an energy-depleted elephant?
RG Boles, EA Zaki, JR Kerr, K Das, S Biswas… – Mitochondrion, 2015
… Herein, we tested for these variants in chronic fatigue, CRPS, SIDS and depression. … CVS = cyclic
vomiting syndrome, Fxn abd pain = functional abdominal pain (a common pediatric functional
syndrome), IBS = irritable bowel syndrome, CRPS = complex regional pain syndrome. …
[HTML] TURAN and EVAN Mediate Pollen Tube Reception in Arabidopsis Synergids through Protein Glycosylation
H Lindner, SA Kessler, LM Müller, H Shimosato-Asano… – 2015
… Abbreviations:: ConA, Concanavalin A; CRPs, cysteine-rich polypeptides; CrRLK1L, Catharanthus
roseus receptor-like kinase 1-like subfamily; DAE, days after emasculation; DAP, days after
pollination; DAPI, 4′,6-diamidino-2-phenylindole; DEFL, defensin-like protein; Dol-P …
Facilitated spinal neuropeptide signaling and upregulated inflammatory mediator expression contribute to post-fracture nociceptive sensitization.
X Shi, T Guo, T Wei, W Li, DJ Clark, WS Kingery – PAIN, 2015
… neuropeptide-dependent nociceptive and inflammatory changes in the hindlimbs of rats similar
to those seen in complex regional pain syndrome (CRPS). Inflammatory changes … inflammatory
mediators contributing to nociceptive sensitization in a rodent fracture model of CRPS. …
Ketamine-A Narrative Review of Its Uses in Medicine.
BM Radvansky, S Puri, AN Sifonios, JD Eloy, V Le – American Journal of Therapeutics, 2015
… pain clinics, and in the prehospital realm. It has been used to treat postoperative pain, chronic
pain, complex regional pain syndrome (CRPS), phantom limb pain (PLP), and other neuropathic
conditions requiring anal- gesia. … CRPS has remained a difficult-to-treat entity. …
Trends in Coronary Revascularization Procedures among Medicare Beneficiaries between Fiscal Years 2010 and 2013
A Kugelmass, MR Reynolds, DJ Cohen, PP Brown… – … : Cardiovascular Quality and …, 2015
… Mortality rates were highest and increasing for MBs presenting with STEMI across all procedures.
Conclusions: The overall volume of CRPs among MBs is declining and more MBs are presenting
with an AMI, and overall mortality rates are increasing year over year. …
CORD STIMULATIONS IN PATIENTS WITH COMPLEX REGIONAL PAIN SYNDROME: A RANDOMIZED PLACEBO CONTROLLED TRIAL
N Kriek, J Groeneweg, D Stronks, F Huygen
… N. Kriek, J. Groeneweg, D. Stronks, F. Huygen Center for pain management, Erasmus MC,
Rotterdam, The Netherlands Objectives: Spinal cord stimulation (SCS) is an effective invasive
therapy to treat neuropathic pain states including complex regional pain syndrome (CRPS). …
[HTML] Diagnostic value of C-reactive protein to rule out infectious complications after major abdominal surgery: a systematic review and meta-analysis
SL Gans, JJ Atema, S van Dieren, BG Koerkamp… – International Journal of …, 2015
… The posttest odds were calculated by multiplying the pretest odds with the positive and
negative LR. Posttest probabilities for a high and a low CRPs were calculated and presented
in a graph for pretest probabilities across the range of 0 to 100 %. …
[HTML] World congress comes to you 7: Yes we can (control chronic pain)
V Bellan
… If you want more information on CRPS you might find what we know about CRPS helpful as
well as these resources by the Royal College of Physicians. You can also read recent research
published by the team and browse through our CRPS blog articles. …
Fibromyalgia
Factors Associated With Time to Diagnosis in Fibromyalgia
G Chodick, D Weitzman, Y Bar-On, V Shalev, H Amital – Journal of Patient-Centered …, 2015
Background/Aims: The diagnosis of fibromyalgia, a chronic debilitating disorder, is
complicated and affected by various factors of the patient and the caregiver. The objectives
of this study were to investigate the time passing from initial complaints to diagnosis and to …
[PDF] Central Sensitization Syndrome and the Initial Evaluation of a Patient with Fibromyalgia: A Review
KC Fleming, MM Volcheck – Rambam Maimonides Med J, 2015
ABSTRACT In both primary care and consultative practices, patients presenting with
fibromyalgia (FM) often have other medically unexplained somatic symptoms and are
ultimately diagnosed as having central sensitization (CS). Central sensitization …
Does low bone density influence symptoms and functional status in patients with fibromyalgia? Observations from rural South India
AS Babu, FM Ikbal, MS Noone, AN Joseph, D Danda – International Journal of …, 2015
Results Low BMD was seen in 81.6%(129/158) of the persons screened. FMS was seen in
37/158 persons, of which 31/37 (83.7%) had low BMD. Conclusion FMS with low bone
density leads to higher levels of pain and a poorer QoL compared to those without FMS. …
[PDF] Walking as physical exercise in Fibromyalgia: An elicitation study from the Theory of Planned Behavior
MÁ Pastor, S López-Roig, Y Sanz, C Peñacoba – anales de psicología, 2015
Abstract: This study is the first phase of the formative research recommended in the Theory
of Planned Behavior for the development of an intervention. Our aims are to identify modal
beliefs about the performance of an exercise pattern in people with fibromyalgia, to test …
… advances in spinal cord and brainstem fMRI provide an unprecedented view of human pain processing and alterations to pain mechanisms in fibromyalgia
R Bosma – 2015
Abstract: Functional MRI of the human spinal cord and brainstem has tremendous potential
to enhance our basic understanding of healthy subcortical function, and impact our ability to
accurately diagnose and treat injury and disease. Despite this potential, there are many …
Understanding High Blood Pressure
S Aziz – 2015
Overcoming Low Self-Esteem with Mindfulness
D Ward – 2015
[HTML] Efficacy and processes of change in acceptance and commitment therapy for chronic pain
M Kemani – 2015
… The first trial utilized a wait-list control condition and included women with fibromyalgia (Study
I). Assessments were done pre- and post-treatment and at 3-month follow-up. … Acceptance and
commitment therapy for fibromyalgia: A randomized controlled trial. …
[PDF] Evaluation of psychiatry consultations requested for inpatients in a university hospital
H Mayda, HI Guzel, Y Gorucu, E Bagcioglu – Bulletin of Clinical Psychopharmacology, 2015
… [Abstract:0282] Psychosomatic disorders Metacognitive evaluation in patients with fibromyalgia
syndrome … In this study, we tested the assumption that patients with Fibromyalgia Syndrome (FMS)
experience more metacognitive thoughts compared to healthy individuals. …
[PDF] Investigation of state and trait anxiety levels among pharmacy students in TRNC
YH Balcıoglu, E Duran – Bulletin of Clinical Psychopharmacology, 2015
… Bulletin of Clinical Psychopharmacology 2015;25(Suppl. 1):S93-S4 [Abstract:0452] Anxiety,
stress, and adjustment disorders Angiotensin-converting enzyme and
methylenetetrahydrofolate reductase gene variations in fibromyalgia syndrome …

by admin | May 4, 2015 | Uncategorized
Anti-Inflammatory Diet Tips for Rheumatoid Arthritis:
Do restaurant meals and snack attacks leave you with rheumatoid arthritis aches and pains? Certain foods – some of your favorites, like steak and cookies – may be causing flareups. Find out what you should stay away from and how to pick tasty substitutes for a healthy rheumatoid arthritis diet…
When you have rheumatoid arthritis (RA), a restaurant menu or open refrigerator can seem like a test: Can you find foods that satisfy your cravings without making joints swell, ache and stiffen?
Definitely. It’s easier than you think. Read on…
You can still eat meat – as long as you choose leaner cuts. Crave salty snacks? Eat nuts instead of chips.
The key is following an anti-inflammatory diet, which helps you avoid RA flares. And these smarter food choices aren’t necessarily boring ones.
Antioxidant-rich fruits and vegetables, high-fiber grains and healthy fats all constitute a rheumatoid arthritis diet that can help you reduce RA aches – in a matter of days.“I start my RA patients on a general anti-inflammatory diet, and they feel better within a week,” says internist Leo Galland, M.D., whose book The Fat Resistance Diet (Three Rivers Press) is based on anti-inflammatory foods.
“Their pain and stiffness is greatly reduced.”
We asked RA experts how to avoid flareups without sacrificing your favorite treats. Here’s what they said:
1. Red meat, pork, poultry, eggs, butter
Why they’re RA triggers: These animal products contain harmful saturated fat, which increases inflammation in the body.
“After a single meal high in saturated fat, blood cells produce more inflammatory signals for several hours,” Dr. Galland says.
“Continue eating like that, and blood cells stay in this inflammatory state,” he adds.
For RA sufferers, that means joint and muscle pain, heartburn, fatigue and even acne.
Anti-inflammatory diet alternative: Love omelets? Whip one up with egg whites (the saturated fat is in the yolk).Proud of your milk mustache? Switch to skim. Can’t give up meat? Choose leaner cuts like sirloin steak, chicken breasts and pork loin chops.
If it’s protein you crave, get it from salmon or mackerel, which are rich in healthful omega-3 fatty acids (you’ll learn more about their health-boosting benefits in the next section).
But “get more fats from plant sources than animal,” says David Rakel, M.D, director of Integrative Medicine at the University of Wisconsin School of Medicine.
“Fat isn’t bad, but we need more polyunsaturated and monounsaturated fats, such as those found in olive oil, nuts and avocados.”
2. Store-bought chips, margarine
Why they’re RA triggers: These snacks and spreads contain trans-fatty acids (TFAs), oils that are chemically processed to make them more solid and stable.
A diet high in TFAs increases C-reactive protein, a marker doctors use to indicate the amount of inflammation in the blood, according to a 2004 Harvard Medical School study published in the American Journal of Clinical Nutrition.
The study showed that TFA-rich foods had a profound effect on inflammatory markers, making them twice as dangerous as saturated fats.“Adding TFAs to the American diet was one of the worst things we could have done. The body requires a lot more energy to break down trans fats, which creates inflammation,” Dr. Rakel says.
TFAs show up in many packaged and processed foods, but they’re easily detected: Just look at the nutrition label.
Since 2008, the Food and Drug Administration (FDA) has required that all U.S. food manufacturers list trans fats.
But watch out: Even if a label proclaims zero trans fats, it’s not necessarily free of them.
Federal regulations allow products containing up to half a gram of trans fat per serving to be labeled as “trans-fat free.”
That means consumers can easily exceed the maximum daily recommended amount of trans fats (1.11 grams) with just three pieces of toast spread with “trans-fat-free” margarine.A safer bet: Stay away from products that include partially hydrogenated oils on the ingredient list; that’s code for trans-fat content.
Anti-inflammatory diet alternative: Nuts and seeds contain omega-3 fatty acids, a healthier fat that reduces levels of C-reactive protein, according to a 2009 study published in the European Journal of Clinical Nutrition.
“When you crave a crunchy snack, dump the chips and scoop up a handful of walnuts, a great source of omega-3,” says Joan Levinthal, a registered dietitian in Woodland Hills, Calif.
Replace margarine with trans-fat-free spreads, such as Smart Balance Omega-3 Buttery Spread, which contains omega-3-rich flaxseed and fish oil.
3. Cakes, cookies, white bread, potatoes and white rice
Why they’re RA triggers: These comfort foods rank high on the glycemic index (GI).
They quickly break down into sugar, making insulin levels rise, which can cause inflammation.In fact, each 10-point increase in a diet’s glycemic status is associated with a 29% rise in C-reactive protein, according to a 2008 Netherlands study published in the Journal of Clinical Nutrition.
“Sugar increases the inflammatory [process],” says nurse practitioner Marcelle Pick, R.N.C., OB-GYN N.P., author of The Core Balance Diet (Hay House) and co-founder of Women to Women, a holistic medical clinic in Maine.
“If you must have something sugary, eat it with some protein to slow its breakdown into glucose.”
Anti-inflammatory diet alternative: By replacing white bread, potatoes and rice with moderate servings of whole-grain bread, sweet potatoes and brown rice, you’re eating on the lower end of the GI index.
Plus, you’re adding more fiber to your diet, which fights inflammation, according to the Arthritis Foundation.
Bing cherries have been found to reduce inflammatory markers, according to a 2006 study in The Journal of Nutrition.Apples and pears are also low on the glycemic scale. Baked and flavored with cinnamon, they’ll taste like a decadent dessert.
“Cinnamon has been shown to help regulate blood sugar; plus, it has a sweet taste all its own,” says registered dietitian Angela Ginn, a spokesperson for the American Dietetic Association.
4. Milk and wheat products
Why they’re RA triggers: Some foods trigger food-intolerance reactions, such as bloating, irritable bowel syndrome (IBS) and headaches.
If you have food sensitivities, your immune system creates antibodies every time you eat them, causing an inflammation cycle, according to Pick.
To prevent this, eliminate foods that disturb your gastrointestinal tract.
Anti-inflammatory diet alternative: Because intolerances differ by person, find out your food allergies first, then pick healthier substitutes.
In month one, Pick’s patients follow a strict month-long elimination diet that excludes common food triggers: sugar, dairy, wheat, eggs, citrus, caffeine, soy. They also keep track of physical reactions in a food diary.In month two, they slowly reintroduce missing foods, one at a time. Any foods that produce a negative reaction are permanently removed from the plate.
“After changing diets, some patients are able to go back to their doctors and ask to be taken off their RA medications,” Pick says.
By Barbara Stanifer, Lifescript

by admin | May 4, 2015 | Uncategorized
You finally sit down to relax at night after a long day at work, and bam! No sooner do you settle into that easy chair that a tightening sensation crawls up your legs, making you get up again. How can you rest when your legs are urging you to move? Here are tips to ease the symptoms of restless legs syndrome, so you can get the relaxation you need…
It feels like your legs constantly want to do the cha-cha, but the cause of restless legs syndrome (RLS) may not be in the lower limbs at all. It actually may be in the brain.
Scientists have found that low levels in the brain of a crucial chemical, dopamine, and a mineral, iron, may trigger the torturous twitching, tingling sensation that’s a hallmark of the disease affecting 10% of Americans.
“Anything that affects the body’s metabolism of dopamine will affect RLS symptoms,” says William Anderson, M.D., an internist who practices sleep medicine at the University of South Florida in Tampa.
That’s one reason scientists recommend therapies that target the brain to ease RLS symptoms, from raising levels of dopamine and iron to distracting the mind.
Here are some tricks you can try ease your symptoms, settle down and relax.
1. Raise levels of dopamine
“The problem is usually the dopamine level in the nerves,” says Lorne Label, M.D., chief of staff at Los Robles Hospital and Medical Center in Thousand Oaks, Calif., and clinical professor of neurology at University of California, Los Angeles.Increasing dopamine will help ease symptoms, he says.
Drugs containing “dopaminergic agents,” such as pramipexole and ropinirole, largely used to treat Parkinson’s disease, increase dopamine and have been shown to reduce symptoms of RLS, according to the National Institutes of Health.
“Folic acid also helps improve production of the neurotransmitter dopamine,” says Suzy Cohen, Lifescript pharmacist, R.Ph., and author of The 24-hour Pharmacist (William Morrow).
She recommends 800 micrograms (mcg) twice daily.
2. Check your iron
Low iron can be the main cause of RLS symptoms, Dr. Label says.
“If your ferritin [the protein that stores the body’s iron] level isn’t above 50 nanograms per milliliter, it’s not high enough,” Dr. Anderson says.
But the problem may not lie just with low iron levels but rather with how your brain processes it.Iron may be poorly absorbed in the brains of restless legs syndrome patients, according to 2003 Penn State University College of Medicine research that showed poor iron uptake in the brains of autopsied restless legs syndrome patients.
The “iron isn’t being delivered to certain brain cells in an effective way,” explains James R. Connor, Ph.D., who led the study.
To check whether you need iron supplements, see your doctor for a simple blood test.
3. Boost your B vitamin intake
“Folate [a B vitamin] increases blood flow (circulation) and, therefore, could improve RLS,” Cohen says.
Folic acid can be taken as supplements or through foods, such as peanuts, garbanzo beans, lentils and spinach in its naturally occurring form, folate.
Another B vitamin, B12, has also been directly linked to RLS, according to Dr. Anderson.
The recommended dietary allowance of vitamin B12 is 2.4 mcg. Ask your doctor if you might benefit from more.
4. Use a sequential compression device (SCD)
A sequential compression device is a mechanical sleeve that fits over the leg and massages it by inflating and deflating with air (much like the armband used to measure blood pressure). It’s usually used to prevent blood clotting in hospital patients, and one small study has shown it may help RLS patients too.
All nine patients who wore a sequential compression device (SCD) for one hour before bedtime every night for three months reported improved social and daily task function and quality of life, according to a 2007 study by the Department of Medicine at the Walter Reed Army Medical Center in Baltimore.
It might work because “the body is capable of only appreciating a limited number of stimuli simultaneously,” the Restless Legs Syndrome Foundation states, implying the sensory impact of the SCD won out over RLS.
5. Exercise
Working out may alleviate symptoms of restless legs syndrome, according to the National Institutes of Health. But don’t overdo it, cautions the RLS Foundation.
Mild exercise, such as walking, light jogging, or yoga, “may help RLS while vigorous exercise can trigger RLS symptoms in some individuals,” explains the RLS Foundation’s brochure, Triggers for Restless Legs Syndrome.
6. Adjust your medication
“Antipsychotics and antidepressants can worsen RLS,” says Winona Tse, assistant professor of neurology at Mount Sinai Medical Center in New York.
“They interfere with the body’s metabolism of dopamine.”
Any medication that blocks dopamine receptors, including anti-nausea drugs used to reduce vomiting, motion sickness and inner ear dizziness, can worsen symptoms of restless legs syndrome, according to the RLS Foundation. So can antihistamines, frequently used to treat colds and allergies.
If you experience an increase in RLS symptoms while taking other medications, see your doctor about alternatives, decreasing the dosage or possibly discontinuing the medication.
7. Don’t try melatonin
Though restless legs syndrome can disrupt sleep, this common over-the-counter sleep supplement won’t help, according to a 2004 Canadian study.
The naturally occurring hormone melatonin regulates your body’s internal clock, or circadian rhythms. Its levels typically increase at night and taper off toward daybreak.
Melatonin also inhibits the secretion of dopamine, which makes it bad news for restless legs syndrome patients. It might increase RLS symptoms in the evening and night, according to researchers at Sacre-Coeur Hospital in Montreal.
8. Take calcium and magnesium
Calcium and magnesium are minerals that aid in the functioning of muscles and nerves, so they may help RLS patients, Cohen says.
“If it’s low, then you definitely need to have your calcium and magnesium within the normal range,” Dr. Label says.
Cohen recommends a daily combination dose of 600 milligrams (mg) of calcium and 200 mg of magnesium.
“But if after 2-3 months there’s been no improvement, it’s not going to help,” Dr. Label warns.
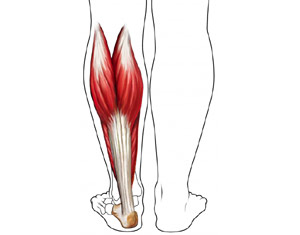
9. Get a massage
Massaging legs before the onset of restless legs syndrome symptoms has been shown to be effective in a 2007 study published in the Journal of Bodywork and Movement Therapies.
It found that therapies such as deep tissue and sports massage for 45 minutes twice a week on the lower extremities reduced symptoms of RLS.
Symptoms were reported to decrease after two treatments and continued to improve over the following three weeks. 10. Run a warm bath (or cold shower)
“Taking a hot bath may relieve discomfort for a [short] time,” Dr. Label says.
However, once you get out of the bath, the symptoms will probably return, he says.
“Others say a cold shower is soothing,” says the RLS Foundation. “Ice packs and heating pads have also been used for relief.”
Whether hot or cold temperatures work depends on the individual, it says.
Other Coping Techniques
The foundation suggests other methods for coping with symptoms of restless legs syndrome in various situations. They include:
- Working the nightshift. Because RLS is tied to the body’s circadian rhythms and worsens at night, it may help to work during the wee hours. By staying active at night, there may be relief during the day.However, check with your health-care provider before changing your schedule: There may be other health consequences to staying up all night, the RLS Foundation says.
- Traveling in the morning. Because sitting still for long periods can be challenging for those with restless legs syndrome, plan a long car ride and air travel for the morning hours. This is especially key for overseas flights or trips that involve a change in time zone, factors that further complicate your body’s natural rhythms.
- Requesting a standing work station. Many variations are available to the standard desk. Many people now work standing, at a podium-like work station. This not only may help RLS, but it also improves circulation throughout the body.
- Staying engaged. Bringing snacks to work or on long trips can distract the mind from the onset of RLS symptoms. For example, eating one popcorn kernel or raisin at a time may be enough. Also be sure to pack enough activities and reading material to stay absorbed during a long trip.
- Quitting caffeine. Although no formal research exists that shows a reduction in caffeine intake can lessen the symptoms of RLS, several patients have reported that quitting the stimulant has helped.
“Caffeine has been linked to an increase in RLS symptoms,” the Restless Legs Syndrome Foundation states. “[It] is present in coffee, tea, chocolate, soda, and other common foods and beverages. Check ingredient listing carefully.”
By Sally Schultheiss, Lifescript

 Many Americans live with chronic pain in one form or another. About 52.5 million Americans report having been diagnosed with some illness that causes chronic pain, like arthritis, rheumatoid arthritis, lupus, gout, or fibromyalgia. The symptoms of chronic pain can be very severe and can dramatically affect a person’s quality of life. Finding relief of pain due to chronic pain syndromes can be tough, but according to Harvard Medical School, tai chi could help.
Many Americans live with chronic pain in one form or another. About 52.5 million Americans report having been diagnosed with some illness that causes chronic pain, like arthritis, rheumatoid arthritis, lupus, gout, or fibromyalgia. The symptoms of chronic pain can be very severe and can dramatically affect a person’s quality of life. Finding relief of pain due to chronic pain syndromes can be tough, but according to Harvard Medical School, tai chi could help.