About a decade ago, Beverly Rzigalinski, a molecular biologist now at Virginia College of Osteopathic Medicine, was asked by a colleague to look into nanoparticles. “Nanoparticles? Yuck,” she thought. She off-handedly told a student to throw them on some neurons growing in the lab and take notes on what happened. She had no hope for the experiment, sure the nanoparticles would kill all the neurons, but at least she could say she tried.
Rzigalinski was given cerium oxide nanoparticles to work with, ten-nanometer wide particles derived from a rare earth metal. (Human hair, by comparison, is 100,000 nanometers wide.) No one had looked at their biological applications, and Rzigalinski was not particularly impressed with their résumé. Cerium oxide nanoparticles’ listed industrial uses included glass polishing and fuel combustion, nothing that seemed promising for neuroscience.
A month and a half later, Rzigalinski noticed the dishes still sitting in the lab’s incubator. She marched straight over to the student, launching into a lecture about not wasting expensive resources on cells that were surely long dead. (Neurons in the lab typically stayed alive for only three weeks.) But the student assured her the cells treated with nanoparticles were still alive. Skeptically, she peered into the microscope and was surprised to find living, flourishing neurons. Rzigalinski has been studying nanoparticles ever since.
Other neuroscientists are joining her, taking advantage of nanoparticles’ unique properties to identify new therapies, shuttle existing therapies into the brain, and examine the brain on a level and depth never before possible.
Recyclable Antioxidants
When treated with cerium oxide particles, Rzigalinski’s neurons survived for up to six months, nine times longer than usual. Cerium oxide nanoparticles may extend life in this way by neutralizing free radicals, unpaired electrons that are highly reactive and can damage DNA. The body’s defenses against free radicals may wear down with time; aging may be due in part to free radicals slowly accumulating unchecked.
Damage induced by free radicals also contributes to a number of neurological diseases. Rzigalinski’s work is revealing how cerium oxide nanoparticles can prevent or reverse this destruction as well. Treating mouse models of Parkinson’s disease with cerium oxide particles rescued the loss of dopaminergic cells, the death of which leads to the disease’s characteristic tremors and slow shuffling gait. Cerium oxide nanoparticles also seemed to halt the free radical-triggered cascade of damage that typically follows traumatic brain injury; after injury, nanoparticle-treated mice had fewer signs of free radical damage and better memories compared to control-treated mice. Finally, when flies were administered nanoparticles following a stroke (in a timeframe analogous to receiving treatment upon arrival to a hospital), the treated flies not only lived longer but also had improved performance on fly-specific tasks, like quickly buzzing to the top of the cage.
Antioxidants like vitamins C and E also sop up free radicals, but each antioxidant molecule only destroys one free radical. As Rzigalinski points out, the advantage of cerium oxide nanoparticles is that, “These nanoparticles are regenerative, so they’ll scavenge thousands, or hundreds of thousands, of free radicals.” Cerium oxide nanoparticles neutralize free radicals by snatching the electrons, shuffling them around, and eventually depositing them as water, restoring the nanoparticles to their original state, ready to abolish more free radicals. This recycling means the nanoparticles will continue working after a single dose. Rzigalinski found nanoparticles present as long as six months after injection in mice and, crucially, toxicity has not been an issue, since the dosage is so low. Single doses, or even low doses, can both prevent harmful side effects and keep costs down.
Cerium oxide nanoparticles are effective because, after injection, they immediately get coated with proteins that help carry them into the heart, lungs, and brain—where they need to be to slash disease-causing free radicals. Not all drugs are so lucky.
Trojan Horses
The trouble with treating brain diseases is the brain exists in a separate world, sealed off from the rest of the body. Cells are tightly packed around the brain’s blood vessels, forming the blood brain barrier, a heavily guarded barricade separating the blood and its contents from the brain and spinal cord. This security system works to keep any bacterial infections and toxins in the blood from getting into the ultrasensitive brain. If small or fat-soluble enough, certain approved entities—like water, gases, alcohol, and some hormones—can leak across the border. Larger molecules require exclusive receptors to allow them through, a unique key that unlocks a particular door and grants them access.
While creating an extra level of protection from diseases outside the brain, the blood brain barrier causes trouble for trying to solve diseases within the brain. It’s a notorious nemesis of drug development, preventing an estimated 98% of potential treatments from getting in. Tomas Skrinskas of Precision NanoSystems—a biotechnology company specializing in delivering materials to cells—lamented, “The blood-brain barrier is probably the trickiest [challenge] there is.”
To overcome this hurdle, one current solution involves flooding the blood with drugs, hoping a small proportion passes through by sheer force of will or strength in numbers. But ingesting lots of drugs can trigger nasty side effects elsewhere in the body. Another way to crack through the defenses is to hack into systems already in place for transporting small molecules. Enter nanoparticles.
While some nanoparticles act as treatments, others play the role of Trojan horse: they pretend to be ordinary, recognized molecules, gain access through special receptors, and sneak the drugs with them as they pass through the restricted entry gates. Nate Vinzant, an undergraduate in Gina Forster’s lab at the University of South Dakota, is using iron oxide to smuggle anti-anxiety drugs into the brain.
When injected directly into the brain, antisauvagine decreases anxiety in rats. However, direct injection into the brain isn’t a feasible treatment option for humans and antisauvagine is incapable of passing from the blood to the brain on its own. To sneak it in, Vinzant attached antisauvagine to iron oxide nanoparticles, which are regularly taken into the brain via specific receptors. When hitched to iron, antisauvagine goes along for the ride because “the brain thinks it’s iron,” Vinzant says. Indeed, typically anxious rats given iron-bound antisauvagine displayed less signs of stress than untreated rats, confirming that the drug made its way from the injection site in the abdomen, through the blood, and across the barrier.
More than just a boon for anxiety treatment, this research is a proof of principle. Other drugs can be tethered to nanoparticles like iron and use the same uptake mechanism.
Remote Controls
In addition to improving treatments, nanoparticles can also help researchers understand diseases and the brain in general. President Obama’s BRAIN Initiative, a program aiming to map the neurons and connections within the human brain, is initially focused on the development of novel technologies that may lead to future breakthroughs. This fall, Sarah Stanley, a post-doctoral researcher in Jeffrey Friedman’s lab at Rockefeller University, received one of the initiative’s first grants to develop technology that uses nanoparticles to control neurons.
Stanley’s goal is to examine a diffuse network of neurons distributed throughout the brain. “We were really looking for a way of remotely modulating cells,” Stanley explains, but existing tools weren’t able to go deep or dispersed enough. For example, one popular new technique known as optogenetics, which uses light to activate neurons, wouldn’t work for Stanley’s project because light can’t penetrate very far into tissue. Another method involving uniquely designed drugs and receptors can’t be quickly turned on and off. So Stanley turned to nanoparticles.
Ferritin nanoparticles bind and store iron, and Stanley genetically tweaked the nanoparticles to also associate with a temperature-sensitive channel. When the channel is heated, it opens, leading to the activation of certain genes.
To generate heat, she used radio waves. Unlike light, radio waves freely penetrate tissue. They hit the ferritin nanoparticle, heating the iron core. The hot iron then heats the associated channel, causing it to open. Stanley tested the system by linking it to the production of insulin; when the radio waves heated the iron, the channel opened and the insulin gene was turned on, leading to a measurable increase in insulin. The nanoparticle is “basically acting as a sensor for radio waves,” says Stanley. It’s “transducing what would be entirely innocuous signals into enough energy to open the channel.”
To optimize the system, Stanley first tested it in liver and stem cells of mice, but she is now moving into mouse neurons, intending to turn them on and off with her nanoparticle remote control. The radio waves’ penetration should allow researchers to use this technique to manipulate cells that are both deep and spread throughout the brain. “This tool will allow us to be able to modulate any cells in any [central nervous system] region at the same time in a freely moving mouse,” Stanley notes.
For now, remotely controlling neurons in this way will only be used in research to discover more about these deep or dispersed networks. But eventually, it could potentially be combined with gene therapy to fine-tune protein levels. For example, in diseases with a mutated or dysfunctional gene, like Rett Syndrome, a developmental disorder causing movement and communication difficulties, gene therapy aims to replace the defective gene. Adding a functional gene isn’t always enough, however, as it must be adjusted to produce the appropriate amount of protein. Controlling the gene with radio waves and nanoparticles would allow doctors to carefully tweak the protein production.
Although that’s a long way off, nanoparticles are claiming their spot in the future of neuroscience. In a press conference on innovative technologies at November’s Society for Neuroscience Conference in Washington, D.C., David Van Essen, a neuroscientist at Washington University in St. Louis, indirectly praised Stanley’s project. “It was really exciting to see earlier this fall that the [National Institutes of Health] has awarded about 50 new grants for some amazing, innovative ideas.” He then went on to introduce Rzigalinski’s research on Parkinson’s disease, mentioning how nanotechnology is a new tool providing hope for reversing devastating diseases.
Neuroscientists may need to temper their excitement, however. Clinical trials for cancer treatments have stalled as some nanoparticles—including iron—have been found to generate free radicals, which can trigger cell death. But a compromise may be possible: iron nanoparticles are also being studied to enhance magnetic resonance imaging (MRI) signals and toxicity doesn’t seem to be an issue so long as the doses are kept low. If the drugs the nanoparticles carry with them are powerful enough, lower doses can be used and harmful side effects prevented.
So far, cerium oxide nanoparticles have avoided this issue, but their relentless crusade against free radicals may lead to a different problem: free radicals are crucial to certain cellular processes, including the regulation of blood pressure and function of the immune system. The question of how much free radical scavenging is too much remains to be answered. But, considering the elevated levels of free radicals in disease, perhaps the nanoparticles will have their hands full lowering levels to a healthy range, let alone reducing them enough to cause trouble.
It’s still too early to know whether nanoparticles will usher in a new wave of clinical treatments, but to many researchers, it’s clear that they show great promise. Rzigalinski, for example, has long since apologized to her student for her disbelieving rant. Small as they may be, nanoparticles have the ability to take on Goliath-sized tasks, bringing researchers deep inside the brain, past its defenses, ready to fight destructive forces in new ways.
BY: Teal Burrell
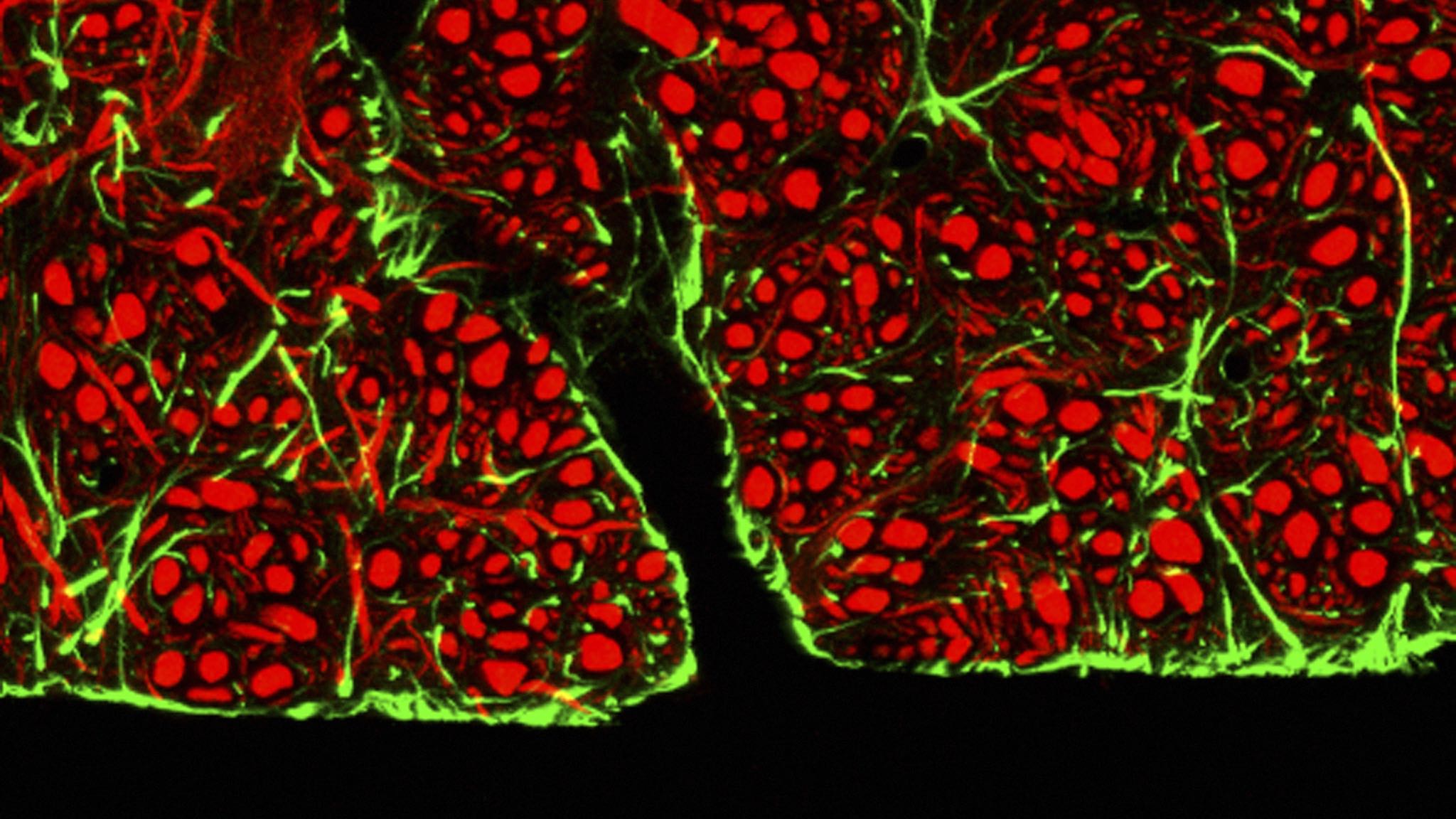
Image credit: C.J. Guerin, PhD/Science Photo Library/Corbis